Final Exam Flash Cards
Remember: It is always about bicarbonate and dialysate mixture.
- You are out of dialysate or bicarb
- Bicarb or dialysate mixed with too much water. Lots of water and less powder mixture means less electrolytes. And conductivity measures the electrical conduction of electrolytes. With less electrolytes, you conductivity will be lower.
- Also if there is an obstruction in the flow of dialysate/bicarb, the conductivity will also be lower. The HD machine is broken. Tell biomed.
- Lowest conductivity = 10
- Dialysate/Bicarb mixed with too little water. There are lots of electrolytes due to more powder mixed with too little water, so conductivity will be higher.
- Machine is broken. Call biomed
- Highest conductivity is 17
- High phosphorus
- Toxins
- A blood clot
- Poor placement
- A fibrin sheath
- fever/chills
- redness
- swelling
- drainage
What to do:
- tell the nurse
- DO NOT START HD UNLESS INSTRUCTED TO DO SO
- Wash Hands
- check the access for signs and symptoms of infection
- Plan where you are going to place the needles so no one area is repeatedly punctured
- Clean the patient’s access to prevent bacteria from entering the blood
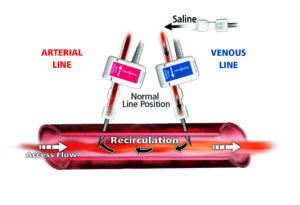
- Insert the needles making sure the venous needle is with the direction of blood flow to minimize recirculation. The arterial needle can be either way
- Separation of lines
- Air or foam in lines/chambers
- Bleeding at the exit sites
- Sudden changes in arterial/venous pressures
- Wash hands
- check for redness, warmth, or drainage
- monitor for fever and chills
- Remember most infections are causes by Staph Aureus, a common bacteria on the human skin
- Should be used for < 90 days due to increased infection risk
- Have higher incidence of infection
- Half of the catheters in the subclavian veins cause stenosis
- Have higher incidence of air embolisms
- Lower infection and complications
- Better patency (open) rates
The disadvantage is that they are harder to create so sometimes the surgeon has no choice but to do a graft
- A needle tip punctures a vessel and goes to the outside allowing blood to seep to the surrounding tissue.
- Assess for infection (redness, warmth, drainage, soreness, needle damage)
- Listen to bruit with stethoscope
- Palpate pulse over the anastomosed vein
- Feel the thrill
- Venous must be antegrade or with the flow of blood
- Arterial can be either way.
- Never flip or rotate needles
- Keep the bevel facing UP
- More likely to thrombose or clot
- DO NOT last as long as fistulas
- Have lower patency rates than fistulas
- But grafts are a good choice with patients have few usable veins for dialysis or poor veins
- You can use it sooner than a fistula
- High-pitched swooshing bruit
- Vascular access recirculation
- Changes in thrill
- some areas of the fistula are difficult to cannulate
- Adjusts feed water temperature to 77 to 82 using hot and cold water to prevent RO membrane damage.
- Also known as the artificial kidney
- Replaces functions of the kidney
- Maintains consistent and stable environment for cell survival
- Filters and removes body waste products
AV fistula
- No food or drinks in refrigerators with blood samples
- Always place used dialyzers/tubing in leak-proof containers. Red bags inside
- Clean all surfaces and dialysis machine per protocol (1:100 EPA-approved bleach solution)
- WE DO A LOT OF CLEANING IN DIALYSIS!

- Uses ultrasonic device to detect air in the blood path
- Present in the post-dialyzer tubing (venous chamber)
- Clamps the post-dialyzer tubing after the venous chamber.

Don’t let predialyzer and post dialyzer tubing confuse you on the test.
Notice that the venous chamber is inside the air detector. Venous line is after the dialyzer or post dialyzer. The venous line must be loaded in order to be clamped when air is detected. It prevents air from entering the patient. This is a critical safety mechanism.
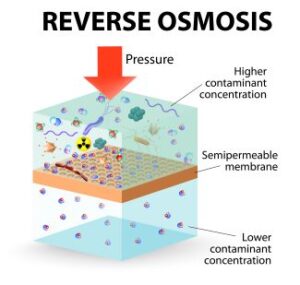
- Hydraulic pressure is used to move water through a membrane.
Microbial or bacteria
- < 200 CFU/mL
- Action level 50 CFU/mL
CFU = colony forming units
Endotoxin
- < 2 EU/mL
- Action level 1 EU/mL
EU = endotoxin units
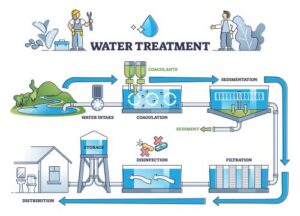
- water softener
- Carbon tanks
- multimedia tank
- brine
- blending valve
- RO membrane
- Alum (binds with particles to remove them. Removes large sediments)
- Flouride (good for our teeth)
- Chloramines (to kill bacteria)
Not added is Zinc
Municipal water has added chemicals that makes it safe for us to use, but these chemicals are not good to use in dialysis patients and must be removed.
fever and chills

- Organics
- Microorganisms
- Inorganics
- Watch for patient’s symptons
- Look at patient’s blood tests
- and of course, do the water testing that you are requires (total chlorine, monthly cultures, checking for water hardness)
Recommends voluntary standards for dialysis water treatment
Oversees the safety and effectiveness of medical devices
- Gases from the atmosphere
- Minerals in the ground
- Pesticides
- Chemicals such as chloramines that are added as required by public health
Our RO system must remove all these contaminants to make it safe
- fever
- chills
- nausea and vomiting
- but mostly fever and chills
Removes calcium and magnesium by ion exchange
Calcium and magnesium makes water “hard”
The brine tank supplies the salt (sodium) used for ion exchange.
- Because patients are exposed to large numbers of water during dialysis
- TCV < 80%
- Label incomplete
- Aesthetic appearance
- It reached the maximum number of uses according to manufacturer
- Must be verified by 2 people
- 2 people are needed to verify that the reprocessed dialyzer has a negative germicide test and that it is the right reprocessed dialyzer for the patient.
- Hepatitis B patients did not participate in dialyzer reprocessing.
- Perform a germicide residual test on the dialyzers (it must be negative)
- Visually inspect the dialyzer.
- Burning sensation in patient’s access
- Swelling of the throat
- Shortness of breath
Think allergic reaction!
- To get initial Total Cell Volume
- To remove residual sterilant
- To remove small amounts of byproducts from the manufacturing process
- Label all chemical containers
- Train employees
- Keep material safety data sheets for all chemicals (MSDS)
Reprocessing adversely affects the clearance rate of the dialyzer
- Sterilant inside a new dialyzer
- Small amounts by cellulose byproducts
- Complement activation and immune response
- Medicare encouraged dialyzer reprocessing due to the changes in the way it paid dialysis facilities. Facilities had to do it to save money.
- The return of blood at the end of the treatment.
- Cerebral edema caused by rapid removal of BUN from the blood
- First symptom of is a headache
- Think neurological symptoms
- Swelling or edema
- pedal edema (feet or legs swollen)
- Hypertension
- Tachycardia
- shortness of breath
- inadequate water treatment (chlorine and chloramines)
- kinked blood lines (as the blood cells pass through the kinked areas, they breakdown)
- Warm dialysis fluid (heat causes hemolysis)
- Clotting of a vascular access
- Least likely to occur in a fistula
- Grafts and catheters are more likley to clot or thrombose.
To treat hypotension during dialysis
- Administer IV fluids (Saline). 100ml
- Place the patient in Trendelenburg position (lower head and elevate legs to increase blood flow to heart and brain)
- 60 to 100 beats per minute.
- < bradycardia
- > 100 tachycardia
Trendelenburg on the left side
Remember that air embolisms are more likely to occur in patients with catheters since catheters are closer to the heart.
- The state achieved when the patient has No edema, no shortness or breath (dyspnea) and blood pressure is normal for the patient.
- Usually a post dialysis weight
- Method of killing most but not all bacteria/microorganisms
- Check needle placement
- check blood pressure (usually happens in low blood pressures)
- Notify RN is not corrected
- trouble breathing
- hives
- itching
- hypotension
- dialyzer membrane tears and allows blood to escape from the blood compartment into the dialyzer compartment.
- Recirculation
- Decreased dialyzer performance due to reprocessing
- Decreased pump speed (BFR)
- Low URR/ LOw Kt/V: extend time, Increase BFR, Increase DFR, better dialyzer.
- Caused by the shifting concentration of SODIUM
- Turn off UF
- Give saline bolus
- Massage
- Apply warmth
- Electrolyte imbalances
- hypotension
- dialysate composition errors
end products of bacterial breakdown
Breakdown of red blood cells with a concurrent loss or liberation of hemoglobin and large amount of potassium.
Toxin produced by certain bacteria
Bradycardia: Heart rate < 60
Tachcyardia: heart rate > 100
12 to 20 breaths per minute
BP should be around 120/80 or systolic blood pressure < 140, so a blood pressure of 145/95 is ABNORMAL
Respiratory rate 12 to 20
Ideal body temp: 98.6 F
Heart rate 60 to 100
- Erythropoetin to make red blood cells
- Calcitriol to activate Vitamin D and absorb calcium
- Renin for blood pressure
- Edema
- Anemia
- Fatigue
- Itchiness
- changes in skin color
- Inability to sleep

Diabetes
Flow in opposite direction or countercurrent flow to increase rate of difussion or removal of waste products
Transmembrane pressure or TMP
Must be < 13 ml/kg/hr to be safe
- Assess for infection
- Assess the surgical incision for healing
- Listen for bruit and thrill
- Do not cannulate unless you have a doctor’s order
- Have larger pores than conventional dialyzers
- Can remove fluid faster
- Remove more beta2-microglobulin
- Can do faster blood flow leading to greater efficiency of removal of toxic substances.
- They can remove broader range of solutes
- They are more expensive
- They are more biocompatible
- They cost more
A number without units that tells you whether the dose of dialysis is adequate
or the prescribed dose of dialysis
must be > 1.2
The most important monitor of dialysis safety
No needle entry. Can be used immediately
Arterial is a negative pressure and venous is a positive pressure.
Remember that predialyzer, post dialyzer, and venous pressures are all positive
It takes a pushing pressure to get blood through the dialyzer and to the patient.
It takes a pulling pressure to remove fluid from the patient.
When going off, dialysate bypasses the dialyzer and it is sent to the drain
Remember that conductivity is a method of checking electrolyte levels in the dialysate (makes sure you mixed dialysate correctly).
- Monitor arterial and venous pressures
- Trap air
- Prevent blood clots from entering patient
Sodium, potassium, glucose, calcium, magnesium, chloride, bicarbonate.
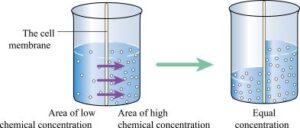
- Diffusion (the movement of particles/solute from high concentration to low concentration)
- Convection (the “dragging” of particles/solute as water moves.
- Adsorption (the adherence of particles to semi-permeable membrane)
Normal saline 0.9%

Water movement from one body compartment to another
- To prevent high blood pressure
- To prevent hypernatremia (high sodium in the blood)
- To prevent edema
- To prevent thirst, which can lead to fluid overload.
- To prevent cardiac arrest
- To prevent Arrhythmias
- Hyperkalemia is a medical emergency because it can cause sudden death.
- Potassium 3.5 to 5.5 mEq/L
- Phosphorus 3.5 to 5.5 mg/dl (sometimes you will see 2.7 to 5.5)
- Calcium 8.4 to 10.2 mg/dl
Both use a semi-permeable membrane
Both use dialysate to help remove waste products
BUT
PD is done daily and HD usually 3x/week
HD uses a vascular access and PD uses a abdominal catheter
- NOT the best choice for every patient. Not all patients are compliance with taking meds daily or have the necessary support system
- There is a shortage of cadaver kidneys
- Mortality is decreasing
- Patients require a thorough medical workup
- Reduces dialysis efficiency
- We can detect it by monitoring of blood (turns very dark).
- Occurs due to stenosis, obstructions, or needles that are too close.
- Same blood that returns to the patient via the venous line comes out of the patient thru the arterial line. Blood never gets the opportunity to go to the heart and lungs so it becomes very dark due to the lack of oxygen
- Extreme muscle weakness and abnormal heart rhythms
Occurs since the kidneys stop producing calcitriol necessary to absorb calcium

- Vitamin Deficiency
- Inadequate erythropoetin
- Indequate treatments
- Iron deficiency

