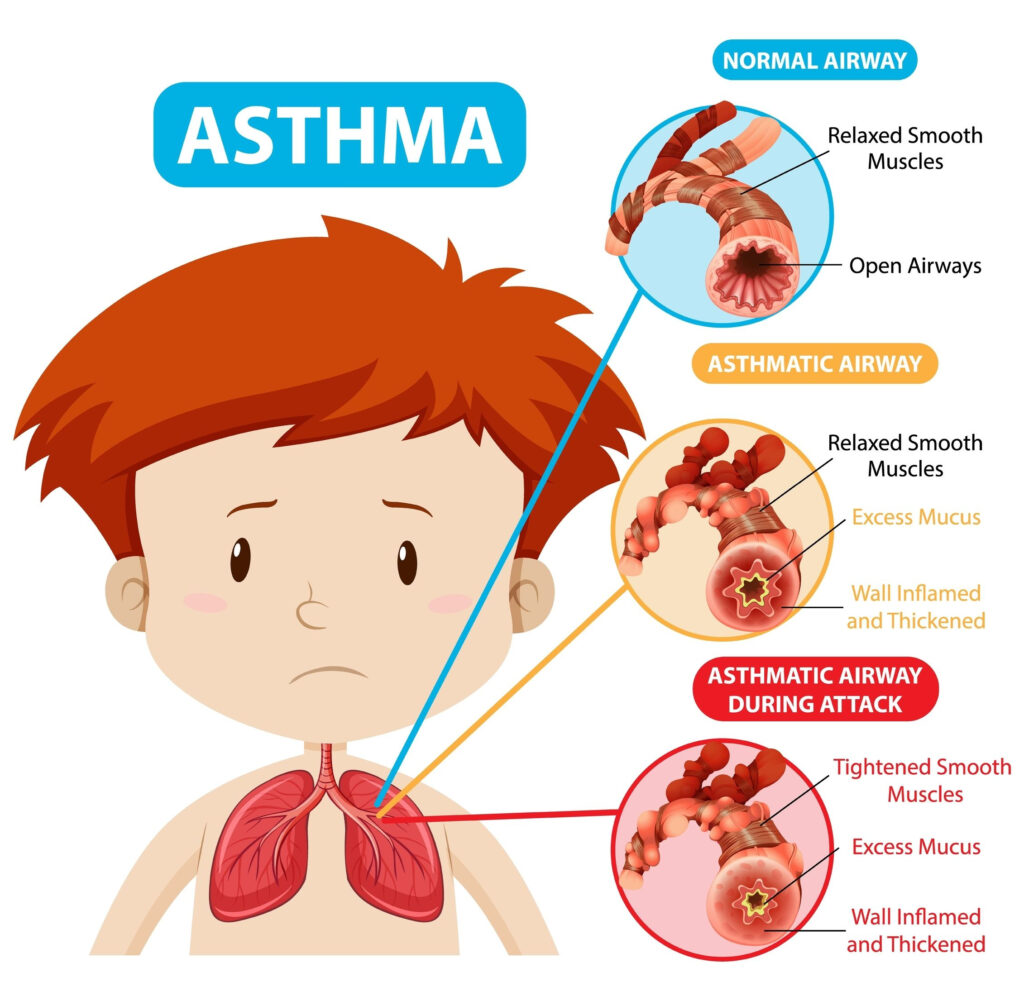
Asthma
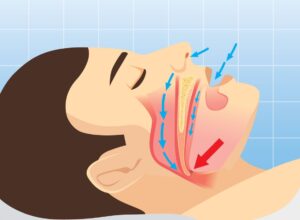
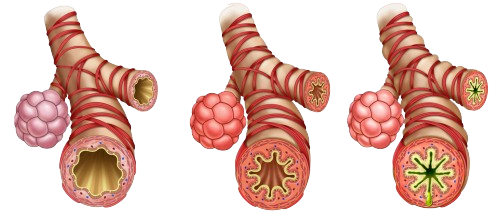
Inflammed, Narrow, Swollen Airways

Causes and Triggers
Genetic, Environment (Pets, Dust, cold, dry air, & smoke), exercise-induced, cold windy weather, cockroaches, Aspirin, NSAIDs such as ibuprofein, ACE inhibitors, Non-selective beta blockers such as propanolol & GERD.

Signs and Symptoms
Dyspnea, Wheezing, tachypnea, chest tightness, coughing, anxiety, mucus, air trapping (retaining CO2).