Disaster Triage, Prioritizing, and Delegation
4 Topics | 2 Quizzes
Neurological System
10 Topics | 1 Quiz
MS, MG, and Guillain Barré
4 Topics | 1 Quiz
The Cardiovascular System
12 Topics | 1 Quiz
Pulmonary System
10 Topics | 1 Quiz
Cushing Versus Addison Disease
3 Topics | 1 Quiz
Thyroid Disorders
2 Topics | 1 Quiz
Parathyroid Disorders
3 Topics | 1 Quiz
DI and SIADH
3 Topics | 1 Quiz
Diabetes
10 Topics | 1 Quiz
Burns
5 Topics | 1 Quiz
Anemias, Aplastic Anemia, Polycythemia Vera, Thrombocytopenia and DIC
9 Topics | 1 Quiz
Cancer, Chemotherapy, Radiation Therapy, and Oncological Emergencies
6 Topics | 1 Quiz
Leukemias, Hodgkin’s Disease, and Multiple Myeloma
4 Topics | 1 Quiz
The GI system
16 Topics | 1 Quiz
Renal and Genitourinary Problems
6 Topics | 1 Quiz
Infection and Isolation Precautions
3 Topics | 1 Quiz
NCLEX Pharmacology
3 Topics | 1 Quiz
TPN, IV Solutions, & Blood Products
6 Topics | 1 Quiz
Lab Values
9 Topics
EKG Rhythms
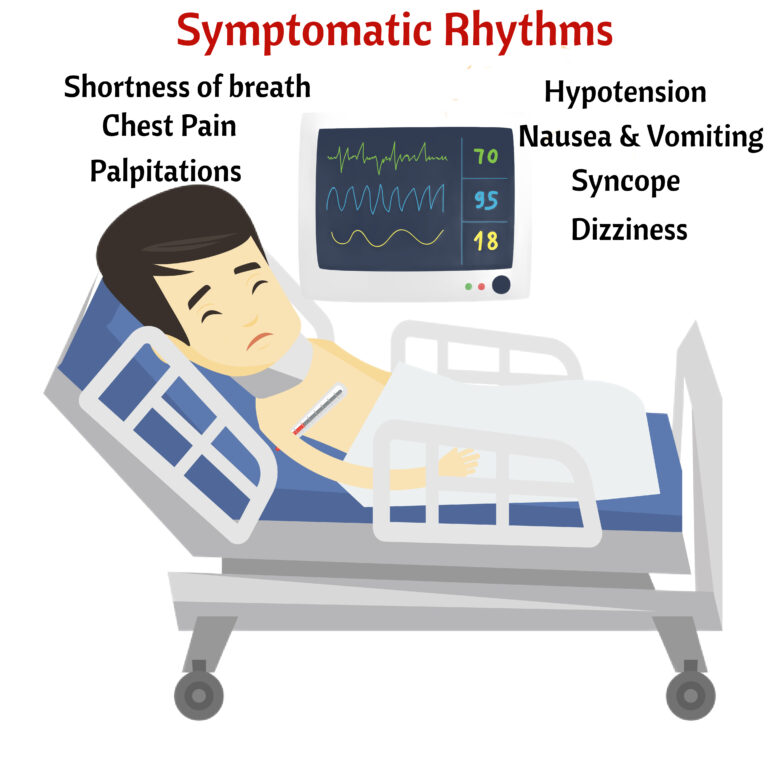
This is what we mean when we say that the client is symptomatic.
Normal Sinus Rhythm
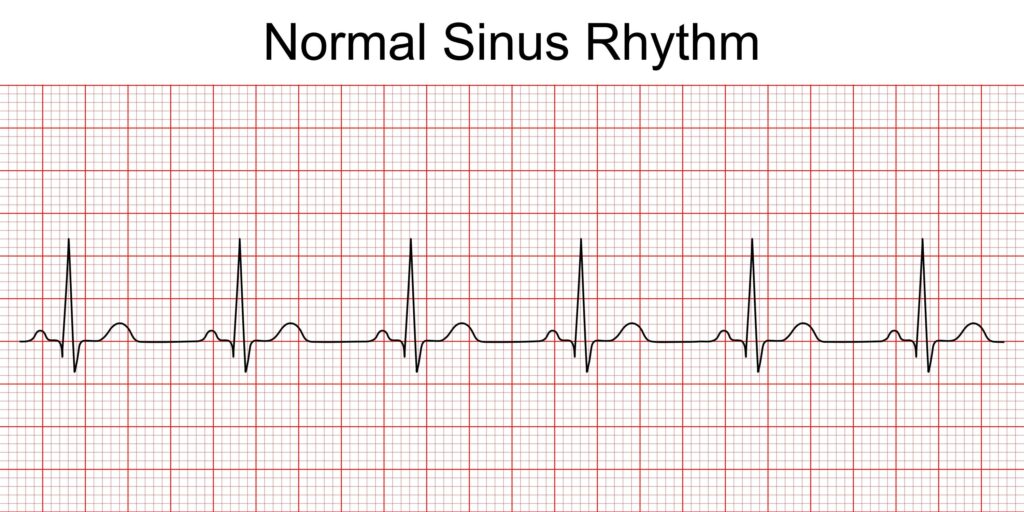
Healthy Rhythm. No Treatment necessary

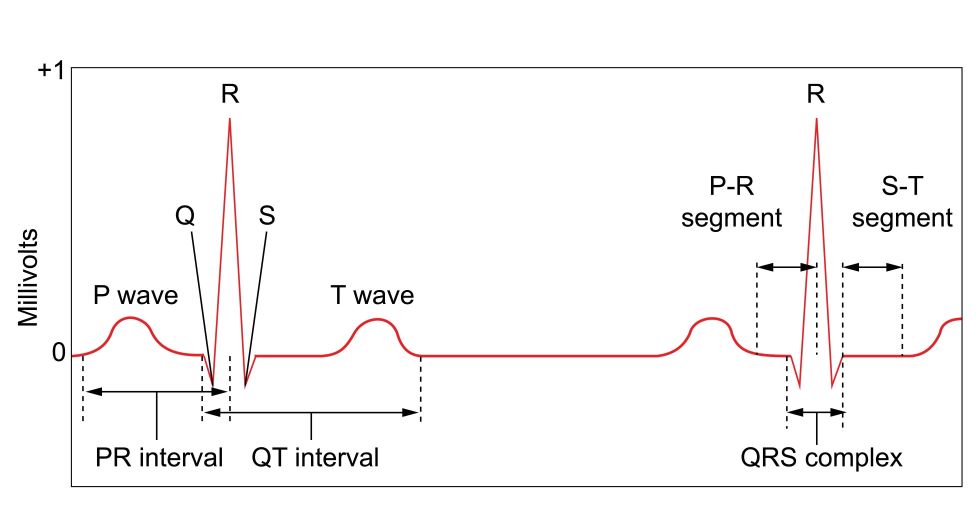
- There should be a P wave for every QRS complex. Check
- All P waves should look alike. Check
- P wave should be measure 0.12 to 0.20.
- Each tiny square is 0.04. One big box is 0.20. A P wave should not be longer than 1 big box.
- QRS complex should measure 0.08 to 0.12.
- To calculate the rate: 300/number of big boxes between QRS complex. Let’s see. There are 3.5 big boxes between each QRS complex. Check. 300/3.5 = 85 bpm is the heart rate.
Sinus Bradycardia
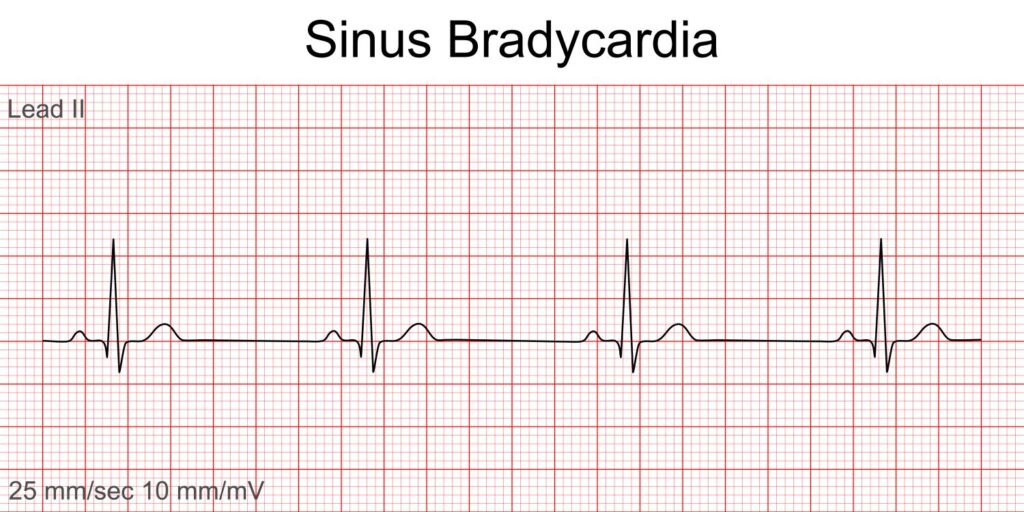
- Normal P wave 0.12 to 0.20 or 3 to 5 little tiny boxes.
- Normal QRS 0.08 to 0.12
- All P waves look the same
- The only difference from Normal Sinus rhythm is the rate < 60
- Is the client symptomatic?
- Symptoms: dizziness, syncope, chest pain, palpitations, nausea, vomiting, and/or dyspnea

- Treatment: Only if symptomatic, otherwise, just monitor. Oxygen, Atropine, Prepare for transcutaneous pacemaker, and treat the cause (MI, hyperkalemia, digoxin or beta blocker toxicity, or hypothermia)
- Asymptomatic bradycardia may need NO treatment
Sinus Tachycardia
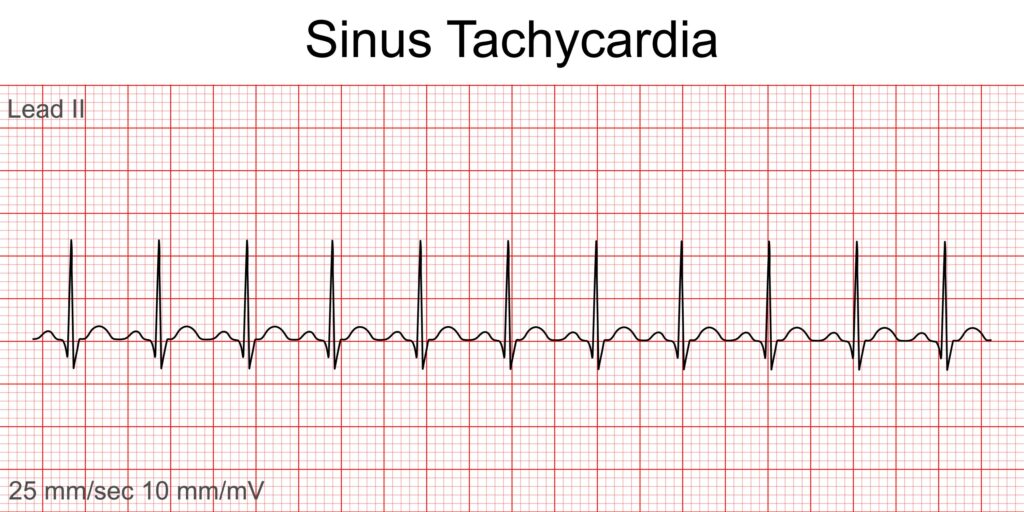
- Everything is the same as normal sinus rhythm except the rate is > 100
- Treat the cause
- Is it pain, exercise, hypoxia, pulmonary embolism, hemorrhage, hyperthyroidism, hypovolemic shock, or fever?

First Degree AV Block
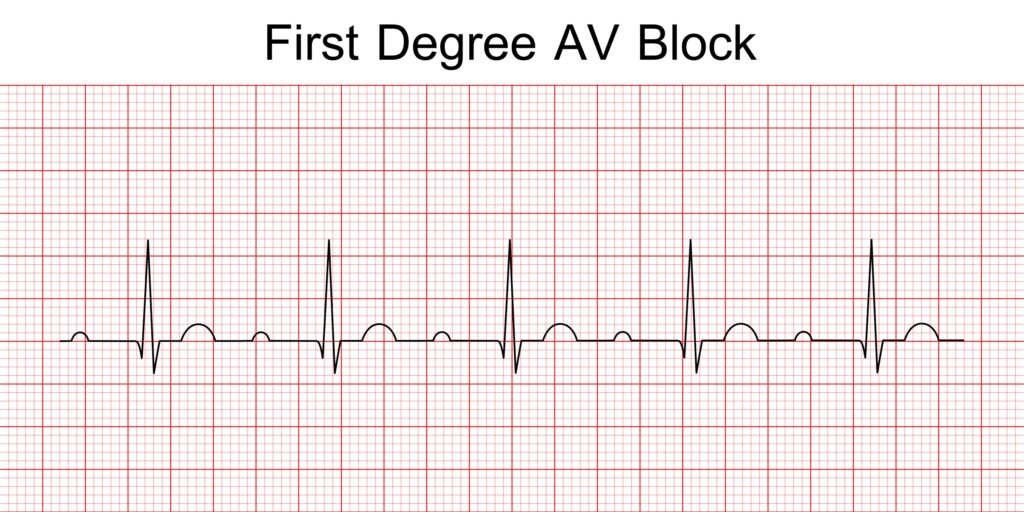
- Everything is normal except for the PR interval is > 0.20. Measure this one= maybe around 0.28
- A P wave that is > 1 big box = first degree AV block
- All P waves and QRS look alike just like NSR.
- Usually asymptomatic
- Treatment: Monitor for advancing block. Be watchful like a predator.
- If symptomatic: treatment is same as symptomatic bradycardia.
Second Degree AV Block Type 1
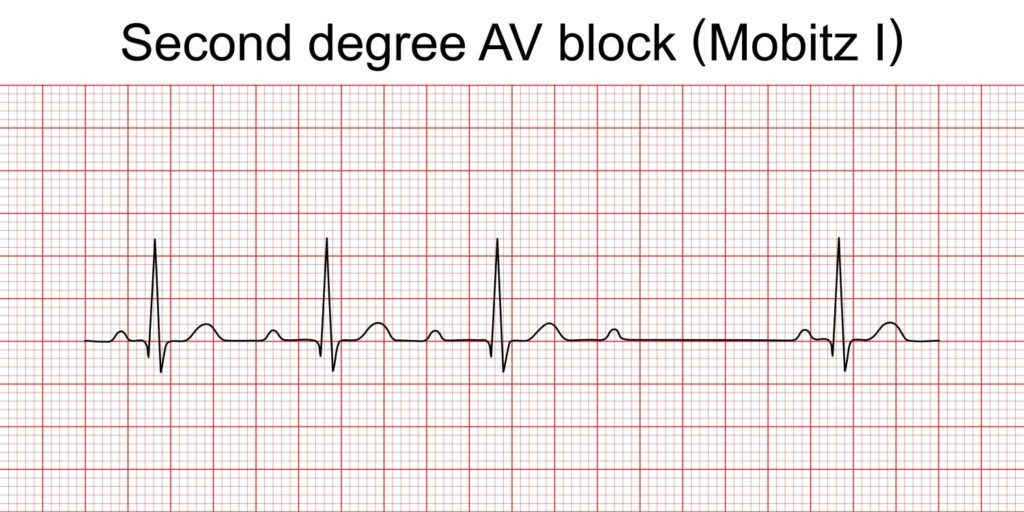
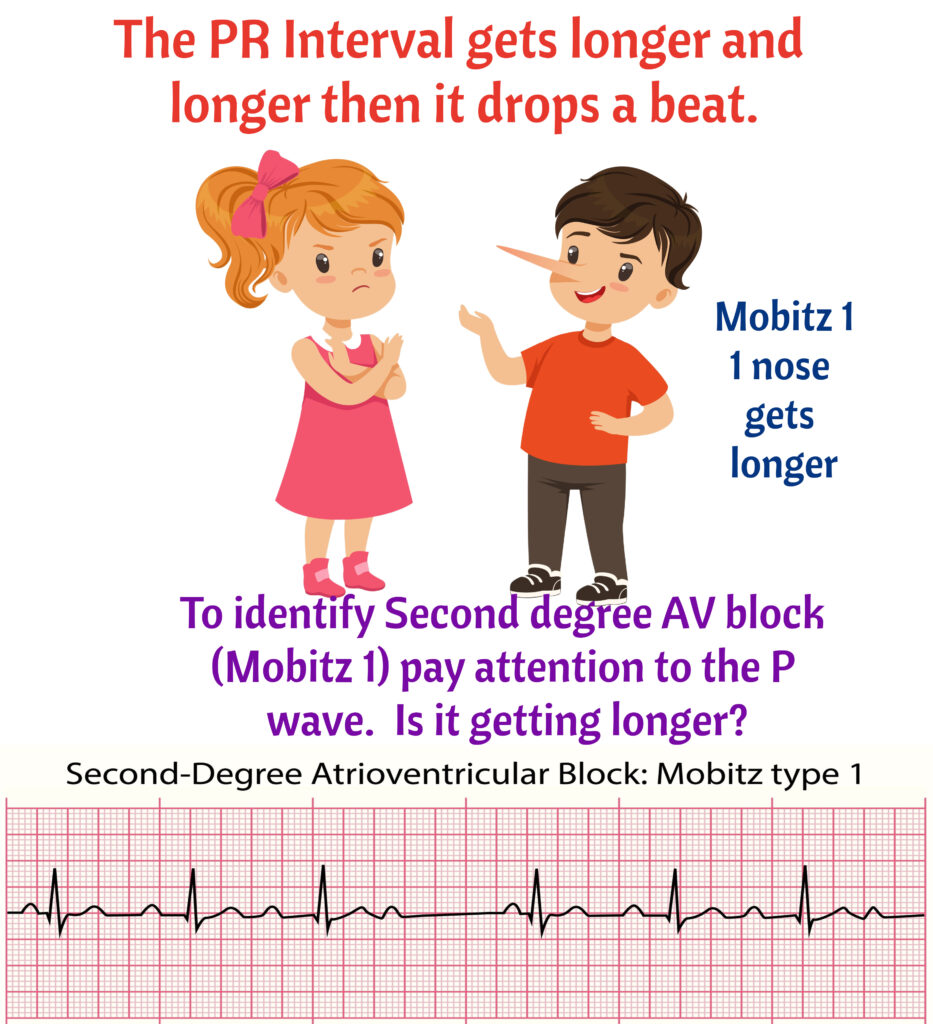
- Also called Mobitz I or Wenckebach I
- The PR interval gets longer and longer and then it gets tired and does not conduct or create a QRS complex.
- Rhythm is irregular due to the dropped beats.
- Some Causes: Digoxin toxicity, heart surgery, & heart attacks.
- Treatment if symptomatic: Oxygen, prepared transcutaneous pacemaker, and atropine
- Monitor for advancing block or symptoms
Second Degree AV Block Type 2
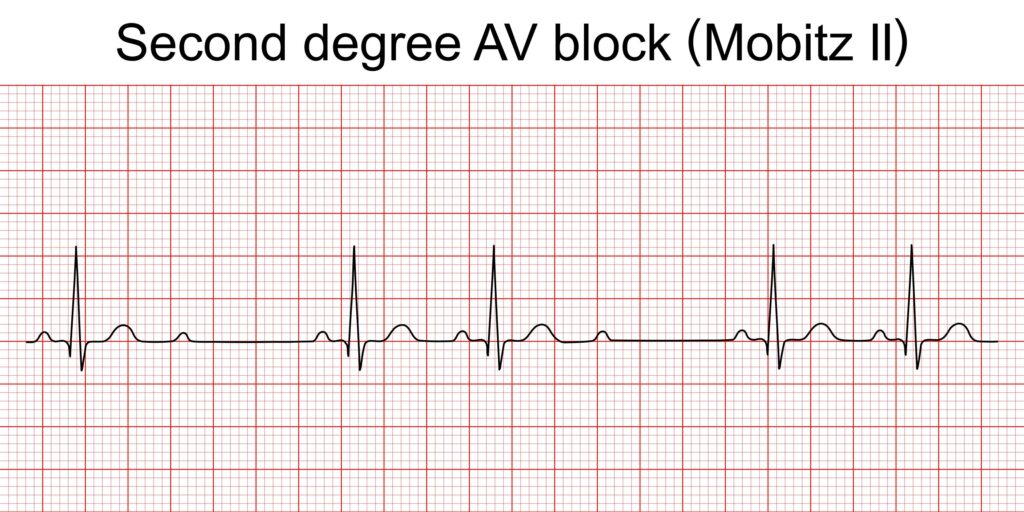
- Also called Mobitz II or Wenckebach II.
- There is a P wave to each QRS, but suddenly no QRS, only a non-conducting P wave.
- Remember, Type I gets longer and longer and Type II P waves are the same.
- Treatment same as Type I
Third Degree AV Block
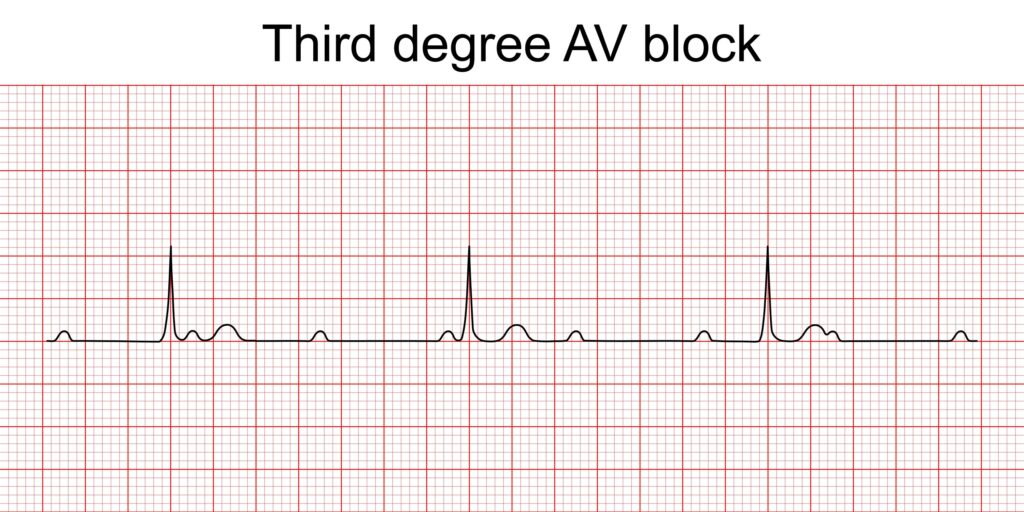
- TOTAL AtrioVentricular Blockage.
- There is no connection between the atria and the ventricles. The P wave and the QRS complexes are doing their own thing.
- Notice that the P waves and the QRS happen are regular intervals. This is a big difference between 2 and 3rd degree AV blocks. Second degree AV blocks look irregular and 3rd degree AV block looks regular.
- Heart rate is usually < 60
- This is a sick, symptomatic client.
- Treatment: Oxygen, Transcutaneous/Permanent Pacemaker, and Atropine.
Atrial Fibrillation
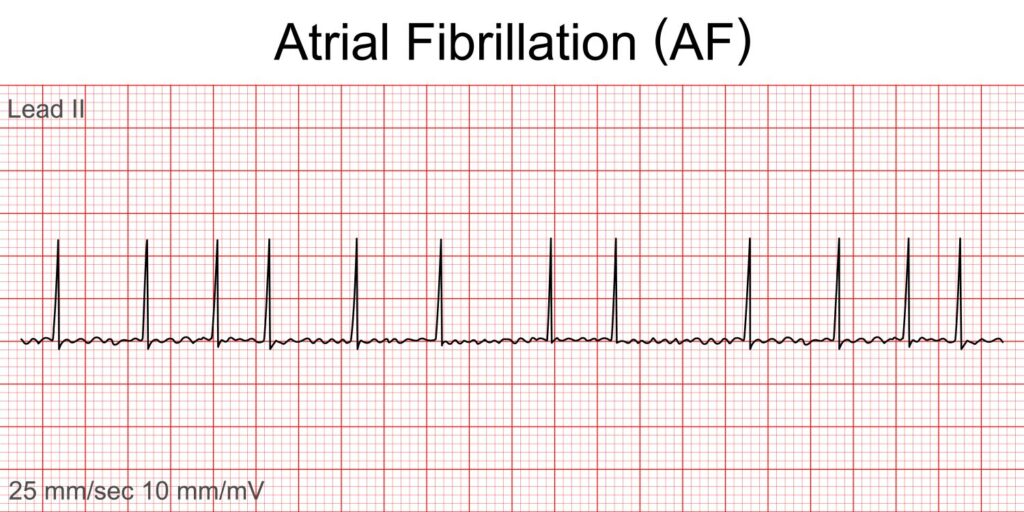
- No identifiable P wave. Fibrillatory waves with irregular QRS complexes. Pulse will feel irregular
- Heart rate > 100 = Uncontrolled Atrial Fibrillation
- Heart rate < 100 = Controlled Atrial Fibrillation.
- Treatment: Antiarrhythmics and Synchronized cardioversion on if symptomatic. Turn on the sync button on the defibrillator when cardioverting this rhythm
- Anticoagulation to prevent emboli if client remains in atrial fibrillation > 48 hours.
- Meds: Amiodarone, Digoxin, Beta blockers, or Calcium Channel Blockers (Verapamil and Diltiazem)
Atrial Flutter
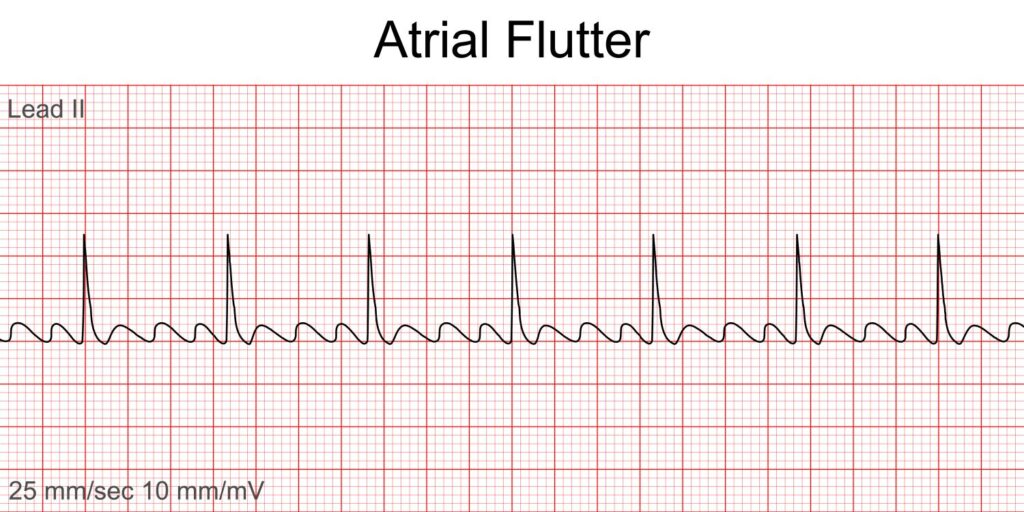
- Flutter waves or “F” waves with a sawtooth appearance.
- This one has a 3:1 conduction or 3 “F” waves to every QRS. Conduction may vary. For example, it can be 2:1. That is, 2 Flutter waves to 1 QRS complex.
- Treatment: same as atrial fibrillation
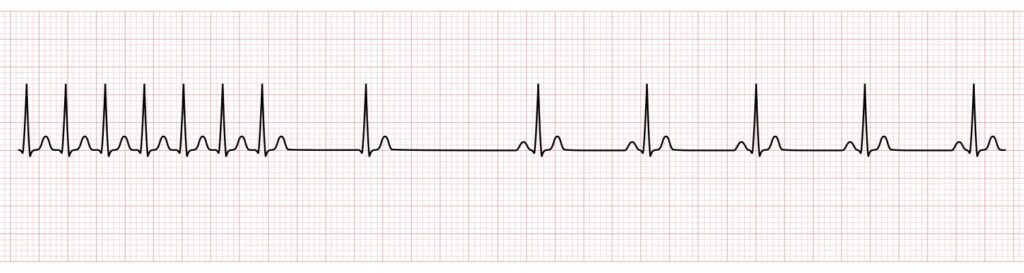
Supraventricular Tachycardia
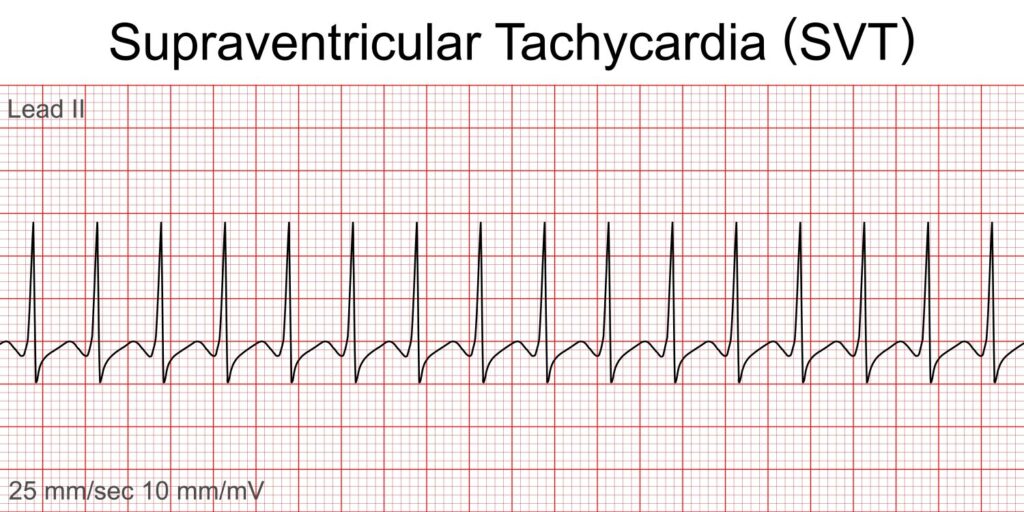
- Fast Narrow complex QRS
- Treatment Adenosine or a calcium channel blocker such as Verapamil and Diltiazem.
- Below is an EKG that shows how Adenosine slows down rhythm.
Ventricular Tachycardia
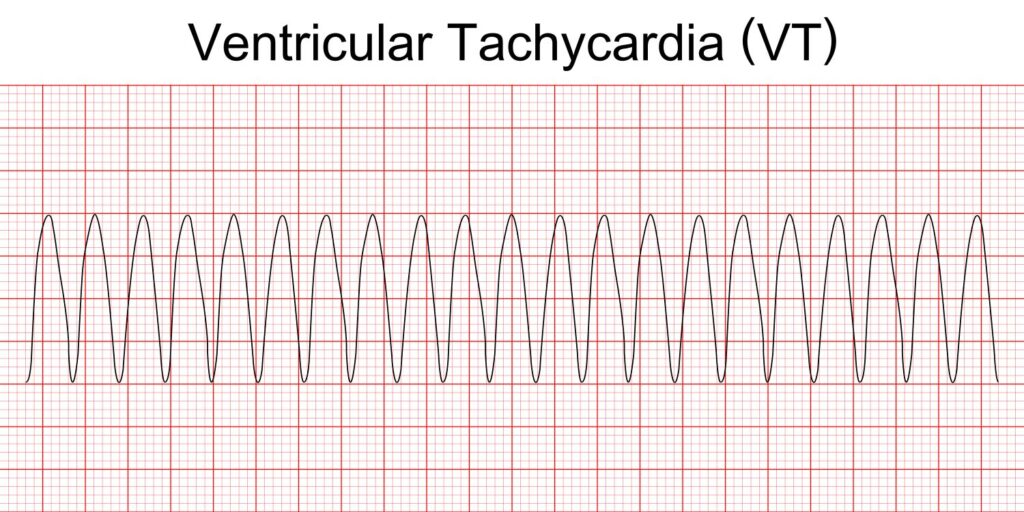
- Irritable ventricle with a rate of 140 to 250 bpm
- Can be paroxysmal (comes and goes)
- Ventricular Tachycardia with a pulse: Synchronized Cardioversion
- Ventricular Tachycardia without a pulse: Defibrillation and CPR
- Meds: Amiodarone, Lidocaine, and Procainamide.
Ventricular Fibrillation
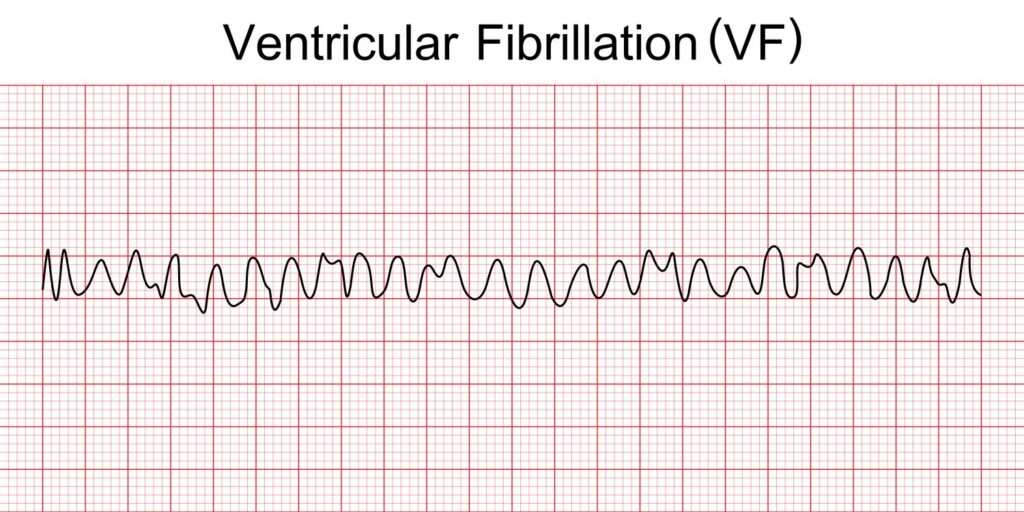
- Assess client to make sure it is not artifact.
- No pulse. Death
- CPR and Defibrillation
- Meds: Epinephrine 1mg IVP and Vasopressin
- Amiodarone 300mg first dose and 150 mg second dose.
- Lidocaine first dose 1 to 1.5 mg/kg and second dose give half of the first dose
