Disaster Triage, Prioritizing, and Delegation
4 Topics | 2 Quizzes
Neurological System
10 Topics | 1 Quiz
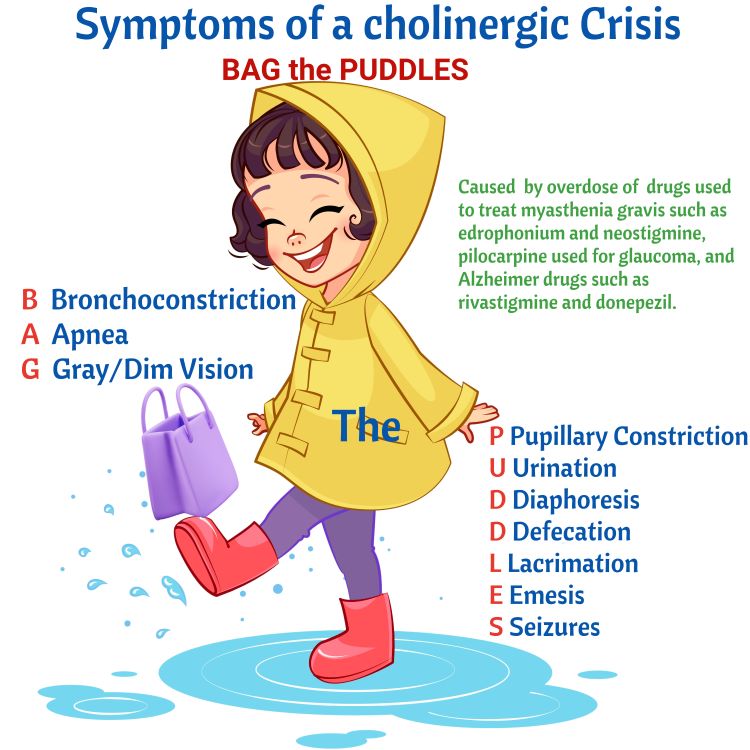
MS, MG, and Guillain Barré
4 Topics | 1 Quiz
The Cardiovascular System
12 Topics | 1 Quiz
Pulmonary System
10 Topics | 1 Quiz
Cushing Versus Addison Disease
3 Topics | 1 Quiz
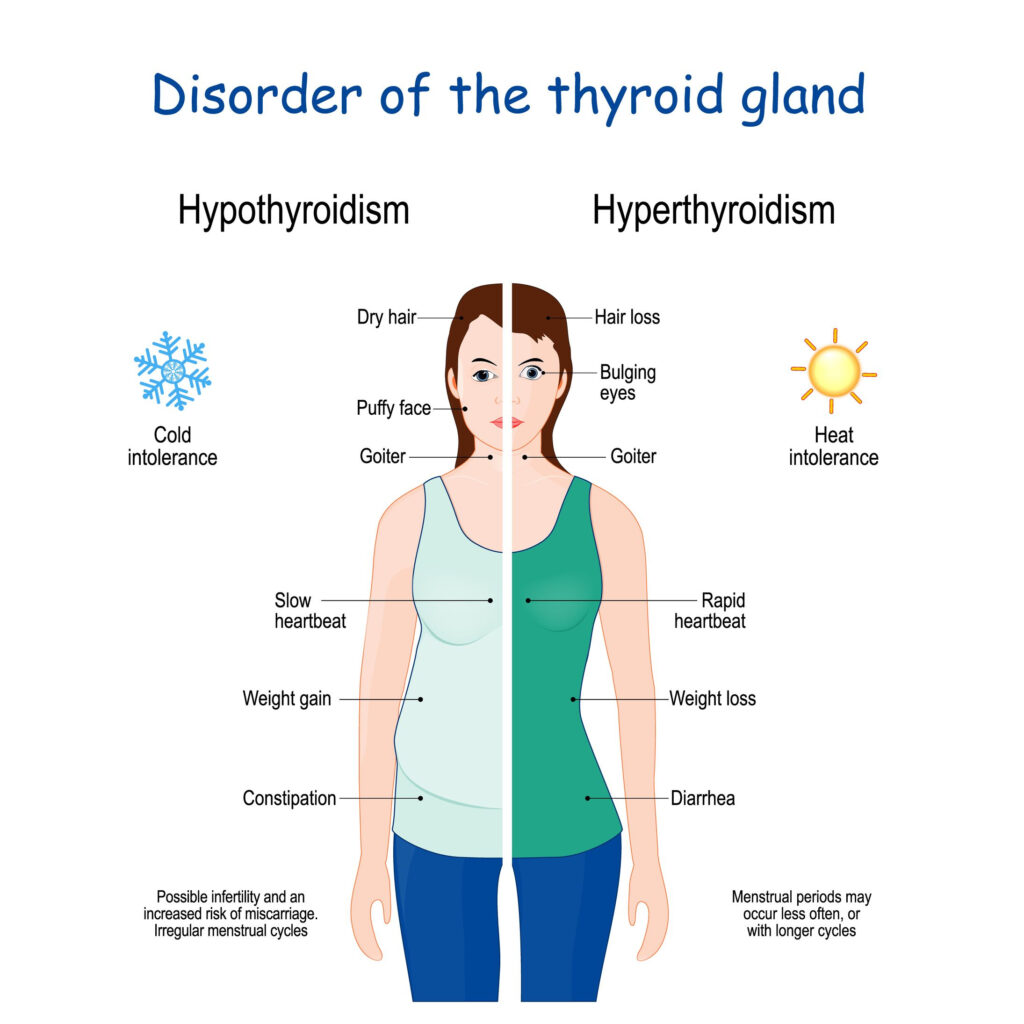
Thyroid Disorders
2 Topics | 1 Quiz
Parathyroid Disorders
3 Topics | 1 Quiz
DI and SIADH
3 Topics | 1 Quiz
Diabetes
10 Topics | 1 Quiz
Burns
5 Topics | 1 Quiz
Anemias, Aplastic Anemia, Polycythemia Vera, Thrombocytopenia and DIC
9 Topics | 1 Quiz
Cancer, Chemotherapy, Radiation Therapy, and Oncological Emergencies
6 Topics | 1 Quiz
Leukemias, Hodgkin’s Disease, and Multiple Myeloma
4 Topics | 1 Quiz
The GI system
16 Topics | 1 Quiz
Renal and Genitourinary Problems
6 Topics | 1 Quiz
Infection and Isolation Precautions
3 Topics | 1 Quiz
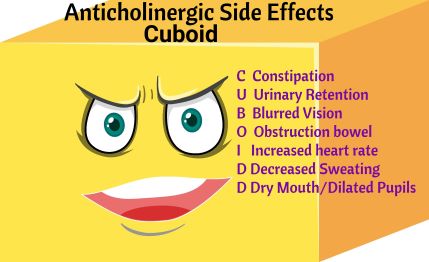
NCLEX Pharmacology
3 Topics | 1 Quiz
TPN, IV Solutions, & Blood Products
6 Topics | 1 Quiz
Lab Values
9 Topics
Famous Drugs
Famous NCLEX Drugs
Click on the headings to expose content. Enjoy these flashcards!

- Ritalin
- For the treatment of Attention Deficit/Hyperactivity Disorder
- Assess for heart-related side effects and report immediately
- Child may need drug holiday due to growth delay

- Inotropine
- It treats hypotension, shock, low cardiac output, and poor organ perfusion
- Monitor EKG for arrhythmias and blood pressure.
- Antipsychotic to treat Schizophrenia
- Blocks dopamine receptors
- Side effects EPS (Extrapyramidal symptoms).
- Akathisia: Feeling restless like you can’t sit still.
- Dystonia: When your muscles contract involuntarily.
- Parkinsonism: Symptoms are similar to Parkinson’s disease.
- Tardive dyskinesia: Facial movements that happen involuntarily.
- Treatment for EPS: diphenhydramine or benztropine.
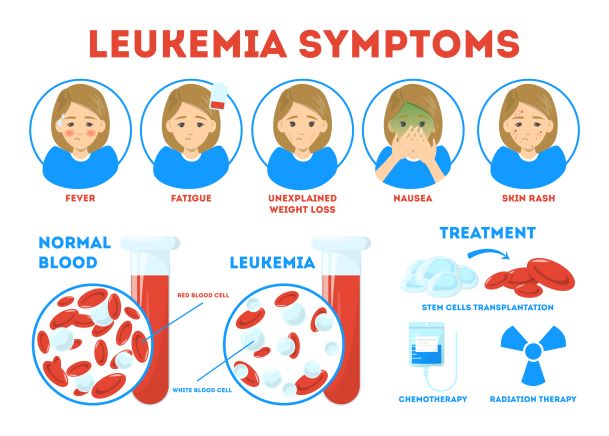
- Treatment for leukemia
- Given IV only
- Monitoring: electrolytes, uric acid, hepatic function, complete blood count with differential, and signs and symptoms of peripheral neuropathy
- Treatment given after menopause
- Estrogen replacement
- Risk of PE, DVT, stroke and MI

- Treatment for scabies and lice
- For scabies: Apply lotion once and leave on for 8 to 12 hours.
- For Lice: Use the shampoo and leave on for 4 minutes with hair uncovered then rinse with warm water and comb with a fine tooth comb.
- Treatment of alcohol withdrawal
- Don’t take with alcohol
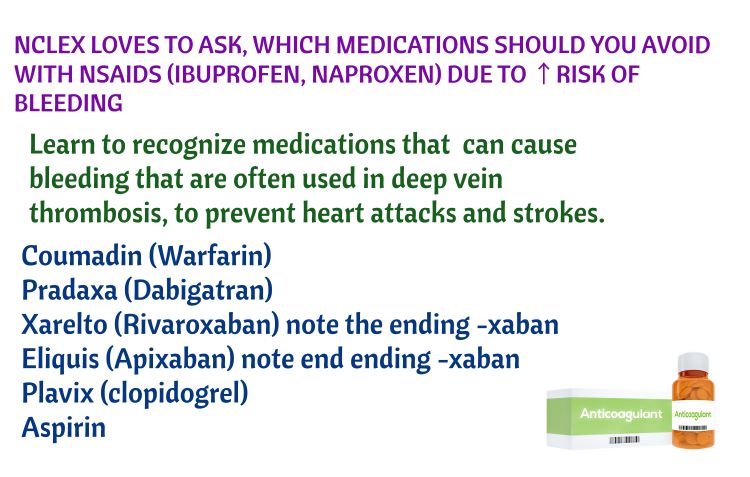
- NSAID
- Treats: Osteoarthritis, rheumatoid arthritis, gout, bursitis, and tendonitis.
- Treats hypothyroidism
- Takes weeks to work
- Take in the morning and on an empty stomach.
- Side effects: think symptoms of hyperthyroidism (anxiety and tachycardia)
- A weak diuretic
- Treats Glaucoma and high altitude sickness.
- This medication can decrease headache, tiredness, nausea, dizziness, and shortness of breath that can occur when you climb quickly to high altitudes
- Do not take if allergic to sulfa
- Sucralfate is a unique anti-ulcer drug. It is a basic aluminum salt of sucrose octasulfate.
- Treats ulcers by coating the ulcer
- Take before meals.
- Bactrim
- Antibiotic for ear infections, bronchitis, pneumonia, urinary tract infections (UTIs), & intestinal infections
- Do not take if allergic to sulfa
- Common side effect: diarrhea so drink plenty of fluids to prevent dehydration.
- Medication of choice for Ventricular tachycardia
- Medication of choice for Supraventricular tachycardia SVT
- Medication of choice for asystole/ bradycardia with symptoms
- Also used to reduce secretions
- Medication of choice for anaphylactic shock
- Medication of choice for bipolar disorder
- Watch for hyponatremia which potentiates toxicity.
- Works for both atrial and ventricular dysrhythmias
- Drug of Choice for Torsades de Pointes and pre-eclampsia to prevent seizures. It is a CNS depressant!
- Reduces nausea
- Do not give in sickle cell crisis due to possible seizures
- GIVE to clients with pancreatitis and avoid morphine. Morphine causes spasms of sphincter of oddi.
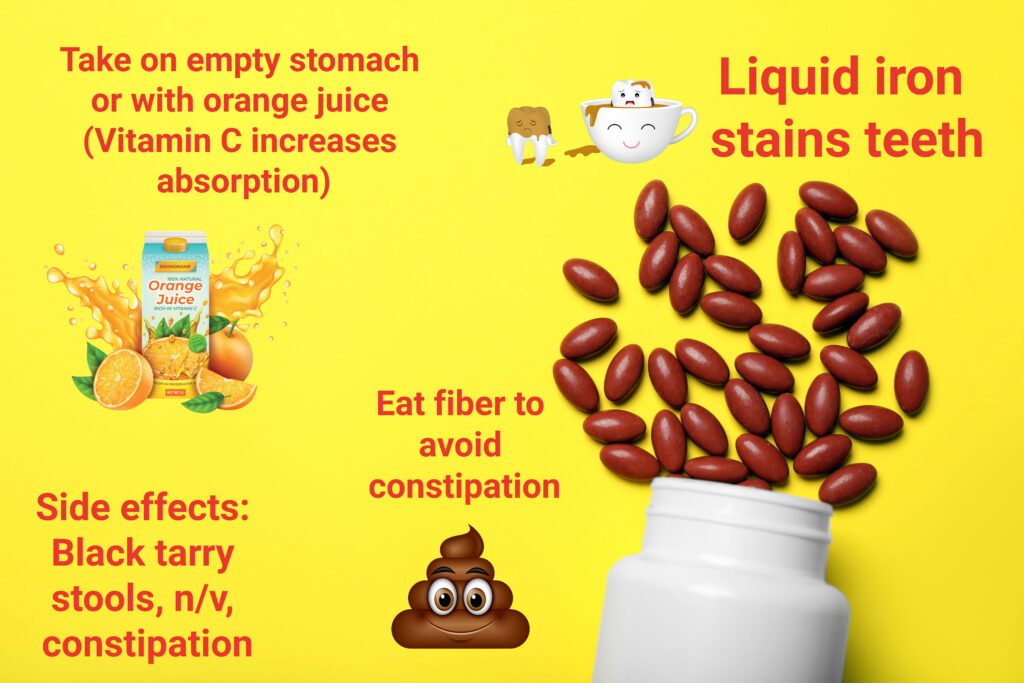
- Use Z track to prevent leakage into SQ tissues. Iron irritates and discolors tissues.
- The oral form discolors teeth-rinse mouth. Give with vitamin C to increase Absorption (orange juice)

- Sublingual give every 5 minutes for chest pain/angina. If no relief after 3 doses, the client is likely having an MI
- Headache is a common symptom because it vasodilates vessels in the brain
- Under 16, do not give aspirin for pain due to Reyes Syndrome (Encephalopathy)
- Educate clients on the potential for bleeding, especially GI bleeding. Report dark, tarry stools
- Too much prednisone, think Cushing: buffalo hump, moon face, hyperglycemia, & hypertension.
- Sample question: A client with Addison Disease has been on Cortisone for a long time. What findings do you expect? The answer is not Addison symptoms but Cushing symptoms.
- Do not stop abruptly to prevent addisonian crisis.
Phenobarbital
- Class: Barbiturate
- Mechanism of action: Increases the effects of GABA, which reduce neuronal excitability by inhibiting nerve transmission. CNS depressants.
- Examples: Phenobarbital, Butalbital, and Primidone
- Problem: Low Therapeutic Index. 10 to 40 mcg/m. Better to use bendodiazepines, which are safer.
- Phenobarbital can be taken during pregnancy but Dilantin is contraindicated.
- Barbiturate withdrawals symptoms: ↑ Temp, restlessness, convulsions, nausea, vomiting, & sleeping problems.
Dilantin
- Treats seizures
- Therapeutic Dilantin level 10 to 20 mcg/mL
- When given IV only use saline. DO NOT use dextrose, it will precipitate.
- Toxicity: ALOC, confusion, nystagmus, & ataxia

Mechanism of action: Inhibit the reuptake of neurotransmitter serotonin by the PRESYNAPTIC neuron.
Uses: Depression, OCD, Anxiety, & PTSD
Examples: Citalopram, Paroxetine, Flouxetine, & Sertraline. (Note the endings, especially -talopram).
Time to work: Symptoms improve within 4 to 6 weeks.
Safety: Avoid taking extra serotonin to prevent serotonin syndrome (MAO inhibitors & St. John Wort).
Side Effects
7 S’s:
Stomach upset (GI upset)
Sexual dysfunction
Serotonin syndrome – incidence increases with other serotonergic agents (i.e. MAOs) – hyperthermia, muscle rigidity, flushing, diarrhea
Sleep difficulties (insomnia)
Suicidal thoughts ( mostly in younger clients)
Stress (agitation, anxiety)
Size increase / Weight gain
Stress (agitation, anxiety)
Size increase / Weight gain
Discontinuation Syndrome: Stomach pain, diarrhea, insomnia, and ataxia. Someone with these symptoms ask: When was your last dose? NCLEX
Serotonin Syndrome (Taking too much or taking with other medications such as MAO inhibitors)


- Mechanism of action: Increases the effects of GABA (an inhibitory neurotransmitted. Think GABA relaxes).
- Uses: Seizures, Prior to an invasive procedure, Anxiety, and insomnia.
- Examples: Alprazolam, Lorazepam, Diazepam (Valium) & Clorazepate. They mostly end with PAM.
- Medication of choice for status epilepticus: Diazepam (Valium).
- Avoid: Alcohol and opioids.
- Toxicity: Bradycardia, repiratory depression, extreme drowsiness, and slurred speech.
- Antidote: Flumazenil
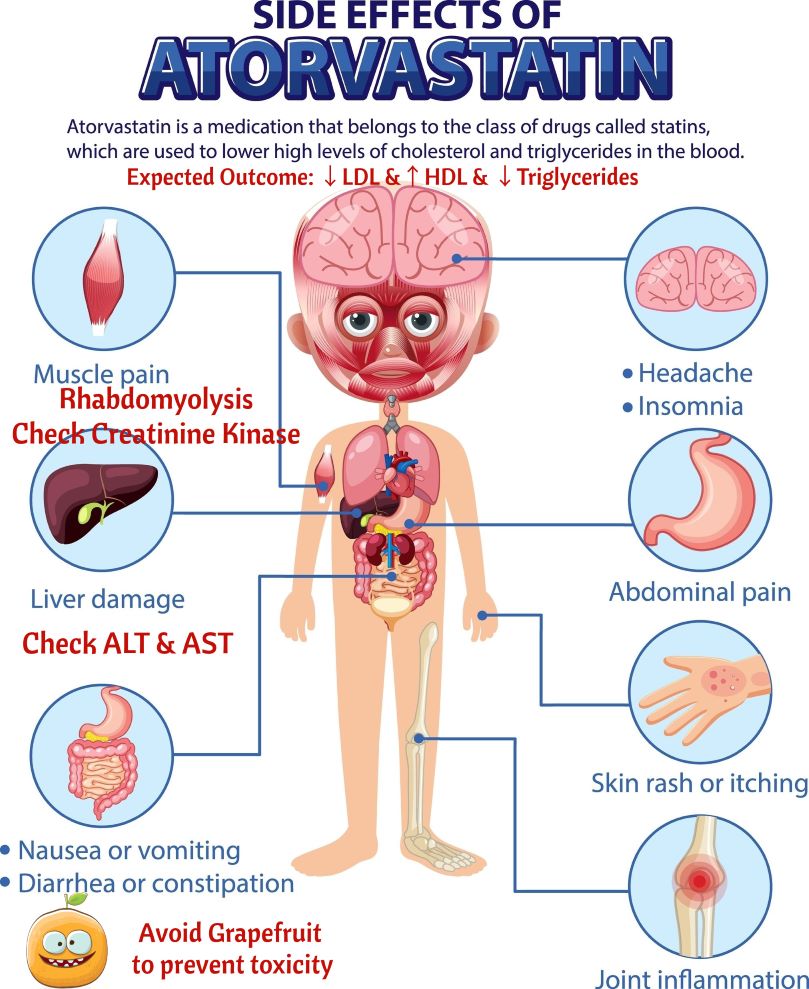
- Mechanism of Action: HMG-CoA Reductase inhibitor. HMG-CoA Reductase is necessary for the synthesis of cholesterol in the liver. With its inhibition, cholesterol is reduced.
- Examples: Known as STATINS. These medications end with -statin: Pravastatin & Simvastatin.
- Goal of treatment: Lower LDL to < 100 mg/dl and increase HDL to > 60 mg/dl. LDL is bad cholesterol and HDL is good cholesterol.
- LDL: fatty substance that sticks to vessels and causes atherosclerosis.
- HDL: fatty substance that removes LDL from the bad to prevent atherosclerosis.
- Side effects:
- Rhabdomyolysis: Breakdown of skeletal muscle. Check Creatine Kinase level.
- Liver Injury: Monitor ALT & AST. Watch for jaundice, abdominal pain in RUQ, and nausea.
- Food interactions: Avoid Grapefruit to prevent toxicity.
- Uses: Lower BP, treat angina, & antidysrhythmics.
- Mechanism of action: Block beta receptors so norepinephrine and epinephrine cannot bind.
- Beta 1 Receptors: Heart and Kidneys.
- Beta 2 Receptors: Lungs & Vascular Smooth Muscle.
- Non-selective beta blocker (affects both heart and lungs): Propranolol- Avoid in asthma.
- Selective Beta Blockers (Only Beta 1): Can be used in asthma since not Beta 2 (Lungs): Atenolol, Esmolol, & Metoprolol.
- Contraindications: Do not use Non-selective Beta Blockers in Asthma. Do not use any Beta Blockers in uncompensated heart failure or cardiogenic shock (Clients with peripheral edema and pulmonary edema).
- Beta Blocker overdose: Bradycardia, hypotension, Dyspnea, ALOC, & 2nd & 3rd degree AV Blocks
- Mechanism of action: Block Calcium Channels in vascular smooth muscle and heart.
- Uses: HTN, angina, and arrhythmias (Verapamil and Diltiazem)
- Examples: Antidysrhythmias: Verapamil and Diltiazem
- Examples: Antihypertensives: Felodipine, Nifedipine, and Amlodipine (Note ending -pine)
- Side effects:
- Constipation: Increase fiber, decrease fat, and increase fluids in diet.
- Gingival Hyperplasia: Good oral Hygiene.
- Hypotension: Monitor Blood pressure
- Safety: Calcium Channel blockers can increase Digoxin Toxicity. Do NOT Eat grapefruit to prevent CCB toxicity.
- Mechanism of action: Inhibit the renin-angiotensin-aldosterone system (RAAS), inactivate bradykinin by breaking it down, and prevent conversion of Angiotensin I to Angiotensin II.
- Angiotensin II: Causes vasoconstriction and increases aldosterole. If it is inhibited, vasodilation and a decrease of aldosterone will occur (↓ Na+ & ↑ K+).
- Again, ↓ SVR and BP, causes kidneys to excrete sodium and water, causes kidneys to retain potassium.
- Examples: the -prils. Captopril, Enalapril, Benazepril.
- Uses: Systolic dysfunctional heart failure, hypertension, and good after an MI.
- Side effects:
- Angioedema: swelling deep in the skin. Very dangerous. Swelling of the face and difficulty breathing.
- Hyperkalemia: Avoid salt substitutes, low potassium diet. Greater risk of hyperkalemia is client is on both spironolactone and an ACE inhibitor. Watch for tall, peaked T waves.
- Persistent cough: Benign. Occurs due to Bradykinin build up in the airways. Teach clients not to stop medication and ask MD to change to another medication.
- Mechanism of action: Prevent Angiotensin II Type I Receptors from binding with Angiotensin II.
- Actions: ↓ SVR, ↓ BP, ↓ blood volume through excretion of sodium and water.
- Again: Vasodilation, Sodium excretion, and Water excretion.
- Examples: end with -sartan. Losartan.
- Uses: Hypertension, Diabetic nephropathy in type 2 diabetes, and heart failure.
- Side effects:
- Cough is rare because do not they do not increase bradykinin build-up in the airways like ACE inhibitors.
- Hyperkalemia
- Like most antihypertensives: Orthostatic hypotension. Change position slowly.
- Do not stop abruptly to prevent rebound hypertension.
- Uses: Infections of the skin, bone, eyes, ears, abdomen and pelvic areas. Kill Klebsiella pneumoniae and Pseudomonas aeruginosa. Target mostly Gram NEGATIVE organisms.
- Mechanism of Action: They are bacteriocidal and inhibit bacteria protein synthesis.
- Administration: Parenteral route mostly since poorly absorbed in the GI Tracts.
- Examples: Vancomycin, Gentamicin, Amikacin, Neomycin, and Streptomycin (Neomycin used to lower ammonia level in hepatic encephalopathy).
- Side effects:
- Renal impairment. Nephrotoxicity. Monitor potassium, BUN and Creatinine, and urine output.
- Tinnitus: ototoxicity.
- Vancomycin- red man syndrome, client turns red if given fast.
- Monitor levels due to nephrotoxicity and ototoxicity:
- Peak: Highest concentration of the medication in the blood. Draw 30 minutes after infusion is complete.
- Trough: Draw immediately before dose is due. Lowest concentration of medication in the blood.
- Mechanism of action: Bactericidal by inhibiting bacteria DNA replication.
- Uses: Bactericidal. Kill Gram POSITIVE bacteria such as Streptococcus pneumoniae. UTIs
- Examples:E Moxifloxacin, Ciprofloxacin, Levofloxacin. Notice the ending – floxacin.
- Side Effects:
- Crystalluria: Flouroquinolones make urine alkaline. Drink plenty of water.
- Prolonged QT interval and Torsades. Especially is given with meds such as Amiodarone.
- Tendon inflammation or rupture (Esp. Achilles Tendon): Report pain swelling, snap feeling or immobility.
- C. Diff: Report Abdominal pain, fever, frequent watery stools to MD and collect stool for C. Diff.
- Do not administer with antacids. Decreases absorption. Give Flouroquinolones and 2 hours later give antacid.
- Mechanism of action: Bacteriostatic. Affect the creation of proteins by bacteria and target subunit 50S on the ribosome.
- Uses: Effective against Gram Positive organisms such as Streptococcal, Chlamydia, Corynecbacterium diptheriae. Treat H. Pylori. Treats C.Diff (Fidaxomicin).
- Examples: Azithromycin, Clarithromycin, & Erythromycin.
- Side effects:
- Prolongs QT interval leading to Torsades. Especially if also taking Amiodarone, Quinine, Quinolones, Doxepin, and Haldoperidol.
- Cholestatic Jaundice: Occurs specially with erythromycin. Elevated bilirubin, Dark colored urine, and Yellowing of the sclera.
- Reversible Ototoxicity:
- Take on empty stomach, with 8 ounces of water. If GI symptoms take with food.
- Mechanism of action: Inhibit bacterial cell wall synthesis and have a beta-lactam ring that binds with penicillin-binding proteins to inhibit cross-linking within the cell wall.
- Examples: Cefoxitin and Cefotetan (2nd Generation). Ceftriaxone, Ceftaroline.
- Uses: Ceftroline (5th generation) treats MRSA. Works agaist infections from gram-positive and gram-negative bacteria. Useful against skin infection, resistant bacteria, meningitis, and other infections.
- Important: Penicillin and Cephalosporins both have a beta-lactam ring so there is cross-sensitivity/allergy risk
- Adverse/Side Effects
- Hypoprothrombinemia: Look for bruising, ecchymosis, bleeding.
- Hypersensitivity reaction: skin rash and pruritis or even anaphylaxis. Discontinue cephalosporin.
- Pseudomembranous colitis and C. Diff: Elevated WBC, fever, watery stool, abdominal cramps, and again leukocytosis.
- Disulfiram-like reaction: nausea, vomiting, flushing, sweating, and headache if alcohol is ingested.
- Warning: Never give Ceftriaxone with calcium solutions because it will precipitate.
Fast Questions Antihypertensives
Fast Questions Antibiotics
Mechanism of Antibiotic Actions
Let's look at some pain medications
Action | Aspirin | Acetaminophen | NSAIDs | Opioids |
|---|---|---|---|---|
Analgesia | ||||
Antipyretic | ||||
Anti-Inflammatory | ||||
Antiplatelet | ||||
Adverse Effects |  BleedingReye's Syndrome |  Hepatotoxicity |  UlcersNephrotoxicity |  RespiratoryDepression |