Endotracheal Tube

Use
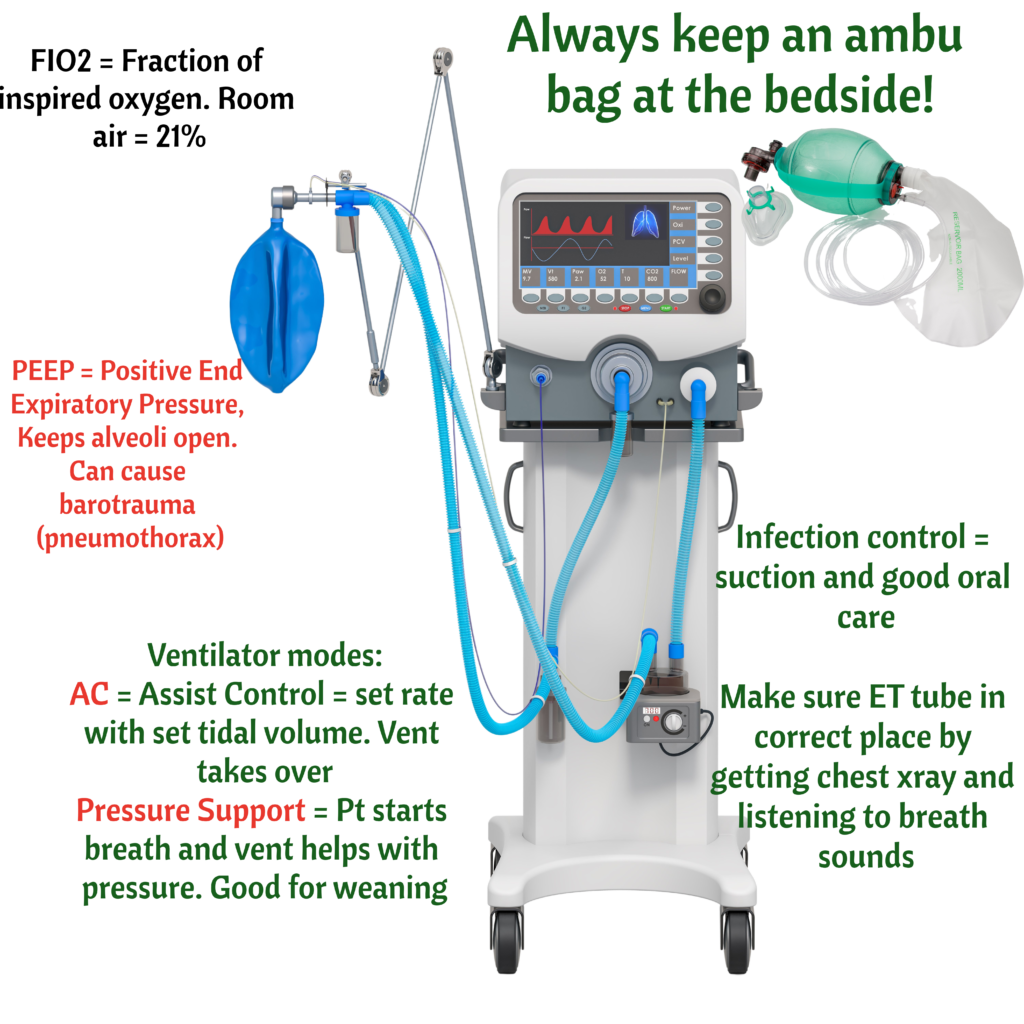
The endotracheal tube used for mechanical ventilation

Airway
It is used to maintain patent airway. Patent airway is always the #1 priority.

Vocal Cords
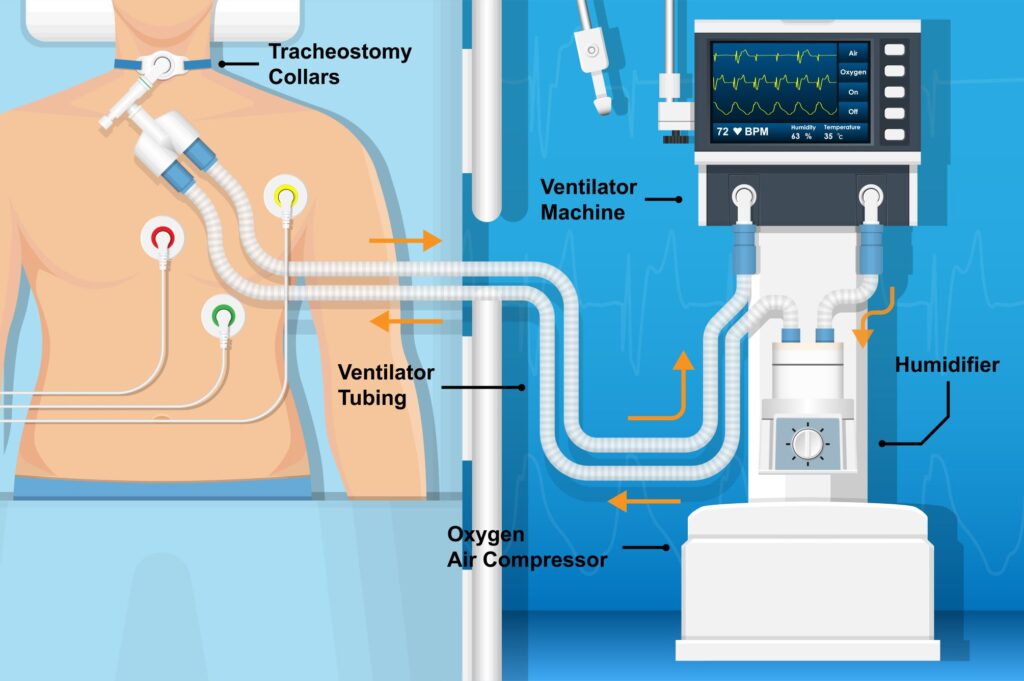
If a client still needs an ET tube (needs mechanical ventilation) more than 10-14 days, a tracheostomy is performed. Why? Protect vocal cords.

X-Ray
Confirm ET tube placement with a chest xray. Priority after intubation? Get a chest xray!

Cuff Pressure
ET tube cuff pressure should be checked every 8 hours and should be < 20 mm Hg.

Problems
Stomach intubation: breath sounds over stomach. ET Tube in right main bronchus = no breath sounds on the left side because ET tube is in the right side of lung.