Disaster Triage, Prioritizing, and Delegation
4 Topics | 2 Quizzes
Neurological System
10 Topics | 1 Quiz
MS, MG, and Guillain Barré
4 Topics | 1 Quiz
The Cardiovascular System
12 Topics | 1 Quiz
Pulmonary System
10 Topics | 1 Quiz
Cushing Versus Addison Disease
3 Topics | 1 Quiz
Thyroid Disorders
2 Topics | 1 Quiz
Parathyroid Disorders
3 Topics | 1 Quiz
DI and SIADH
3 Topics | 1 Quiz
Diabetes
10 Topics | 1 Quiz
Burns
5 Topics | 1 Quiz
Anemias, Aplastic Anemia, Polycythemia Vera, Thrombocytopenia and DIC
9 Topics | 1 Quiz
Cancer, Chemotherapy, Radiation Therapy, and Oncological Emergencies
6 Topics | 1 Quiz
Leukemias, Hodgkin’s Disease, and Multiple Myeloma
4 Topics | 1 Quiz
The GI system
16 Topics | 1 Quiz
Renal and Genitourinary Problems
6 Topics | 1 Quiz
Infection and Isolation Precautions
3 Topics | 1 Quiz
NCLEX Pharmacology
3 Topics | 1 Quiz
TPN, IV Solutions, & Blood Products
6 Topics | 1 Quiz
Lab Values
9 Topics
Prioritizing: Who is the priority client?
Let's learn how to prioritize
To determine who is the sickest client, the NCLEX prioritizing questions follow formats similar to these:
- There is an emergency situation, which client should the nurse assess FIRST?
- At the beginning of the shift the nurse gets report on 4 clients. Which client should the nurse see FIRST?
- The home health/community nurse is visiting 4 clients today. Which client should the nurse visit FIRST?
- The charge nurse is making assignments for the day. Which client should the charge nurse assign to the experienced Registered Nurse?

Think ABC in that order at all times.
It’s all about ABC (Airway, Breathing, and Circulation). If ABC is not helping you determine which patient has priority, then think: Is the problem expected of the disease/condition or is it unexpected or a possible complication? The EXPECTED or UNEXPECTED strategy will be covered after we do ABC.
Airway, Breathing, & Circulation

Here are some AIRWAY problems











BREATHING Problems





CIRCULATION Problems






Expected or Unexpected (A complication)
UNEXPECTED Symptoms/Complications
- Give priority to clients with unexpected symptoms that are life-threatening or represent a serious complication that compromise ABC.
- Try to answer this question to understand what an expected and an unexpected symptom is.
- Never forget, that yes, all clients need to be seen. All are sick. All need you and you will see all, but which one will die sooner if you don’t see him or her right this minute.
- The client on insulin drip has no life-threatening emergency. Blood sugar is elevated, but the client is receiving treatment. EXPECTED (Hypoglycemia; however, would be a complication of treatment and would have priority because it affects the brain).
- Back pain in an abdominal aneurysm= rupture (circulation). UNEXPECTED/COMPLICATION
- Client’s with COPD are expected to have lower saturations and be short of breath with activity. EXPECTED
- The client with pancreatitis is EXPECTED to be in pain.
- Remember: Do not make assumptions. Do not assume that a client with CHRONIC obstructed pulmonary disease with low saturations is in acute respiratory distress.
- NCLEX Must-Know: Back pain in an abdominal aneurysm = rupture. Rush them to surgery!
- Vomiting in a client with esophageal varices is UNEXPECTED because it’s a sign of a serious complication (RUPTURE/BLEEDING). If this client has not ruptured, the increased pressure of vomiting may lead to rupture.
- Pain is EXPECTED in sickle cell crisis. It’s important to treat pain, but saving a client who can bleed out is priority.
- Blood in the stool of a client with Crohn’s disease is EXPECTED.
- Client’s with pneumonia (an infection) are EXPECTED to be febrile.
- A client on skeletal traction is EXPECTED to have pain. Please don’t think that maybe pain is due to possible nerve damage, especially when you have a patient with decreased perfusion to the leg.
- A fasting blood sugar of 80 mg/dl is normal. EXPECTED
- Tidaling in the water seal of a chest tube is EXPECTED. Bubbling in the suction chamber is EXPECTED. However, bubbling in the water seal would be UNEXPECTED (=air leak). By the way, intermittent bubbling after chest tube insertion due to pneumothorax is EXPECTED. Air is coming out. Memorize these.
- Decreased pulses after a cardiac cath is UNEXPECTED. It’s a CIRCULATION problem. Notify the physician or the client may lose an extremity. By the way, decreased perfusion to an extremity always comes up. Look for pulses 1+, pale or cool fingers/toes or numbness and tingling. Pay attention to baselines! Did the extremity have a pulse of +1 before cath lab? Or do both extremities, the affected extremity and the unaffected extremity, have pulses of +1.
- NCLEX Must-Know: Nausea/vomiting in esophageal varices = potential rupture
- NCLEX Must-Know: Decreased pulses, numb toes, cool toes after a heart cath are a priority.
- NCLEX Must-Know: Tidaling in the water seal of a chest tube is EXPECTED. Bubbling in the suction chamber is EXPECTED. Bubbling i the water seal is UNEXPECTED (=air leak) unless it is intermittent bubbling after chest tube insertion due to a pneumothorax. Remember that air needs to come out somehow.
- A client admitted for dehydration is expected to be a little tachycardic. Please don’t begin to think hypovolemic shock when you have the bleeding client with a distended abdomen as a better choice. A client with a heart rate of 102 won’t die if you see him in 15 minutes. EXPECTED
- A client with a bowel resection is not expected to have a fever. UNEXPECTED. But let’s see if there is someone with a greater priority. A post-op fever can wait a little. Confused! Ahhh! Now you are thinking: this expected/unexpected strategy is not perfect or doesn’t work all the time. Nothing is black and white. Here is what critical thinking comes into play. Choose the client with an unexpected/complication problem that relates to ABC.
- A client with a chest tube to suction is EXPECTED to have bubbling in the suction chamber. That’s normal.
- A client with an appendectomy and a distended abdomen likely has post-surgical bleeding. UNEXPECTED. This is a circulatory problem. It has priority over an infection. By the way, make sure you know that BLEEDING/HEMORRHAGE is the number 1 post-surgical priority (of course, unless airway and breathing are compromised). Most people choose pain when asked what is the number 1 post-surgical priority. Be a hero and choose HEMORRHAGE.
- A client with osteomyelitis has an infection. Nausea is often expected.
- Itchiness is common in clients with chronic renal failure due to elevated phosphorus/toxins; however, if a client receiving a blood transfusion or medications such as antibiotics is itchy, think potential allergic reaction. This would be a priority client. Stop the blood or antibiotic or whatever the client is getting. That’s the answer on the NCLEX. Stop the infusion.
- The client with chest pain is potentially having a myocardial infarction. Remember, MI is a priority. Unless you have a client with a compromised airway or not breathing. See them first and then move on to the heart attack.
- A client with chronic renal failure is EXPECTED to be anemic. Usually hospitals do not transfuse unless hemoglobin is < 7.0 mg/dL. There is no mention that the client is symptomatic.
- A client with chronic renal failure is EXPECTED to have an elevated creatinine (and BUN).
- A client with an infected diabetic ulcer is EXPECTED to have an elevated WBC.
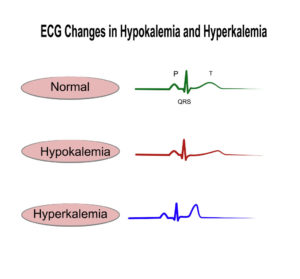
- A potassium of 7.0 mg/dl is hyperkalemia. Hyperkalemia is a deadly lab. It can stop the heart. UNEXPECTED/COMPLICATION. Go save this client! Let me tell you, if a choice has a client with hyperkalemia, I bet you that is your priority cient.
Unstable
- If an answer choice describes the client as UNSTABLE. Think no more…This is likely the PRIORITY client.
- If the “unstable” word is not in the answer choice then what makes a client unstable?
- Hypotension
- ALOC
- Bleeding. Here it is again!
- Abnormal heart rhythms such as heart blocks.
- An abnormal deadly lab such as low blood sugar and hyperkalemia.
- All the ABC problems!
- Too obvious, I hope. The word unstable is in the question.
- Let’s try the next one.
- Nausea is a common side effect of most medications, not just hydrocortisone.
- The client with asthma is still having air exchange (the client has wheezing). If the client had decreased breath sounds it means that the client’s respiratory passages are about to close down or closed down. The client may go into respiratory arrest any second. However, wheezing and a respiratory therapist at the bedside is reassuring.
- The hypotensive, tachycardic, difficult-to- arouse client is UNSTABLE.
ACUTE over chronic
- Simple. Acute problems have priority over chronic problems.
- The client with acute appendicitis has priority over the client with a myocardial infaction who was admitted 7 days ago and will be discharged the next day.
- The client with acute vomiting has priority over a client with COPD.
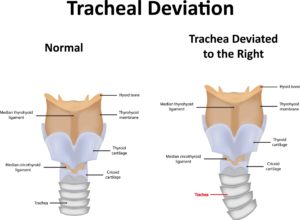
- The client with an acute severe headache has priority over a client with chronic obstructive pulmonary disease (even when COPD is respiratory and you were taught “airway, breathing” first). A severe headache may be a ruptured cerebral aneurysm! Bleeding or a brain bleed/stroke affects ABC!
- The client with an elevated BP has had it for at least a day. Not an acute problem.
- The client who pulled out his NG tube did it 5 hours ago. If it was not a priority 5 hours ago, it is definitely not now.
- The client with sudden chills has an “acute” change in condition. You may say, but wait a minute, we just had a client with a potential infection, with a fever and that client was not a priority client. Well, in that scenario the client was not priority because someone was sicker, but here, in this question, this client is the one with an acute change in condition. Critical thinking! So sepsis/infection may not be a priority in some scenarios because there may be a client with an ABC problem.
Allergic Reactions

- Allergic reactions can vary from simple hives to anaphylaxis (closing of the airway). Prioritize symptoms of allergic reactions.
- And remember, if a client is having an allergic reaction during a medication administration or blood transfusion, the first action is TO STOP THE INFUSION.
ALOC or SHOCK

Shock...not that shock
- Just to emphasize!
- ALOC, signs and symptoms of shock such as tachycardia, hypotension, diaphoresis, decreased pulses, and pallor have PRIORITY in most scenarios.
- I hope you think this is obvious by now.
- A new postoperative client has priority over clients who have been in the hospital for a few days, unless, of course, their condition has changed and have become unstable.
- Also, clients that require temporary monitoring such as a client who had sedation/anesthesia during a procedure (bronchoscopies/EGDs) have PRIORITY.
NEW ADMISSIONS
- New admissions have priority over clients who are ready to be discharged.
ALARMING or MALFUNCTIONING equipment

- Equipment such as ventilators, pacemakers, or IV pumps with critical meds are priority. If a cardiac monitor is alarming, go see that client first. He or she may be in cardiac arrest or other deadly heart rhythm. If an IV alarm is beeping and the patient is getting a caustic medication (a medication that burns skin if it infiltrates), go see that client. Some medications that can cause necrosis are chemotherapeutic agents.

The Simple Terms
- Airway
- Breathing
- Circulation
- Unexpected Symptoms
- Chest Pain
- Deadly Labs
- Unstable
- Bleeding
- Acute over chronic
- ALOC
- Shock
- New post-op
- New Admissions
- Malfunctioning or alarming equipment that is life-saving (e.g. ventilators).
Famous Priority clients
Abdominal Aortic Aneurysm with back pain
Aneurysm ruptured. Client is about to go into hypovolemic shock. Rush to surgery.
Alarming Ventilator
Oh no, the client's respiratory status has been compromised.
Appendicitis who is now pain-free
Think, inflammation causes the pain. Appendix ruptures so pain goes away, but deadly peritonitis is about to start.
IV pump beeping of a client on chemo
Yes, it is infiltrating. Get ready for skin necrosis.
Guillain Barre with shallow breathing
Guillain Barre: Monitor breathing!
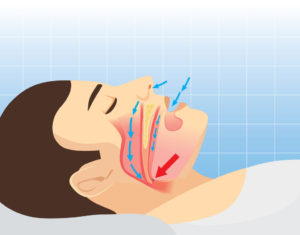
Stroke client eating and coughing
Yes, he is is aspirating!
A cold, pale, decreased pulse extremity
A client with a cast, a broken bone, post-heart cath with an extremity with compromised tissue perfusion is a priority.
Nasogastric tube client who is vomiting
Think Aspiration! It's respiratory
Esophageal Varices Vomiting
If esophageal varices rupture, the client will bleed out.
Tuberculosis client without a mask
The confused tuberculosis client out in the hallway without a mask, coughing on everyone.
