
Notify the physician
If you have assessed a problem that requires a physician’s order or intervention, the answer is to notify the physician.

If you have assessed a problem that requires a physician’s order or intervention, the answer is to notify the physician.
If you are given an assessment then you are looking for an intervention. E.g., a client in severe respiratory distress needs the intubation tray at the bedside first. Assessing respiratory status is not necessary anymore.
If an immediate nursing intervention can improve the client’s condition such as elevate the head of the bed to improve breathing, that’s the answer! Of course, the second priority is to notify the physician of the change of condition.
What is the most important intervention that will save the client’s life if done FIRST! A client with an opioid overdose requries Narcan to start breathing again and not oxygen!

Choose an assesssment. E.g., a client complains of right elbow pain. Notifying the physician without an assessment is silly. What happened? Accident? How long? Is the elbow swollen?
Choose an intervention. An overdose is a problem. How can we reverse the overdose? With an reversal agent. We don’t need an ABG. Even Oxygen will not help if the client is not breathing.

You are told that the client has overdosed. Do not choose assess respiratory status. Give reversal agent. Opioids (Heroin, morphine, fentanyl) give Narcan/Nalaxone. For benzodiazepines give Flumazenil (Romazicon)
Here we have a list of famous priorities. It is not comprehensive. As you encounter more, write them down and memorize them

Click on the titles to expose the priority.
What to do first if this happens.
Place client in left Trendelenberg. Left side with head lowered
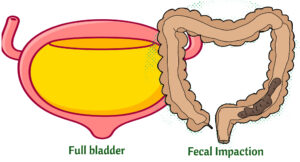
Sit up in bed to decrease blood pressure. Check for bladder distension or fecal impaction. Remove any noxious stimuli.
Autonomic Dysreflexia is an overactive autonomic system in which the client experiences severe hypertension and bradycardia. It is usually due to a spinal cord injury.
Assess for muscle weakness and check potassium levels.
Check potassium levels and digoxin levels. Hypokalemia potentiates digoxin toxicity. If a client has visual disturbances (e.g., seeing halos) and GI symptoms such as diarrhea always think digoxin toxicity. Normal digoxin level is 0.8- 2.0 ng/mL
Too much antidiuretic hormone. Client retains fluid. Client is hyponatremic (dilution from too much fluid). Priority is to restrict fluids
Have the external/transcutaneous pacemaker at the bedside
Priority is to stop the infusion.
Report black-colored stools= GI bleeding
Priority is to check breathing. Remember that paralysis/weakness starts from the lower extremities and moves up the body. The client will go into respiratory arrest/distress as the breathing muscles become weaker/paralyzed.
Don’t do any activity that would further decompensate client such as getting the client out of bed. Keep unstable clients in bed. Also, never feed a client who is having trouble breathing.
Check Blood sugar
Get intubation tray. Any client in respiratory distress, get ready to intubate is almost always the answer.
