Pressure Sores
Risk Factors

Trudy is critically-ill in the intensive care unit. Let's see what makes her at risk for pressure ulcers and what you should do about it as a nurse.
Shearing and friction
Use a draw sheet
Malnutrition
TPN, Tube Feedings. and oral supplements when ready. Vitamin C, Zinc, Carbs, and protein.
Dehydration
Simple! Keep hydrated
Fecal/Urinary Incontinence
Good pericare. May need a foley or a rectal tube to keep skin clean.
Advanced age
She is lucky she is young
Chronic Conditions
Lucky she is not DIABETIC
Casts, restraints, and tracton devices.
Assess skin under these devices
Risk Assessment Braden Scale
- Sensory Perception
- Moisture
- Mobility
- Nutrition
- Friction and Shear
- Very High Risk: Total Score 9 or less
- High Risk: Total Score 10-12
- Moderate Risk: Total Score 13-14
- Mild Risk: Total Score 15-18
- No Risk: Total Score 19-23
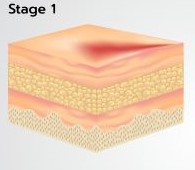
- Intact skin with nonblanchable redness
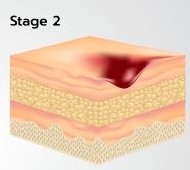
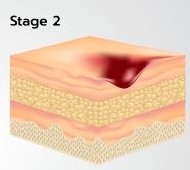
- Loss of dermis
- Red-pink wound bed
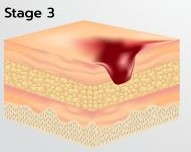
- Full-thickness tissue loss with subcutaneous fat visible.
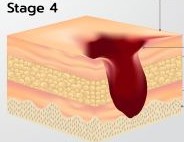
- Full-thickness tissue loss with bone, tendon, or mucleexposed.
- Undermining or tunneling may be present.
Treatments
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Nursing Priorities
- Assess skin especially over bony prominences
- Turn every 1 to 2 hours
- Pressure relieving mattresses
- Avoid shearing/friction
- to skin by using lift sheets.
- Heels off bed
- HOB elevated < 30 degrees is possible
- Use mild soap to cleanse skin.
- Moisturize skin and apply barriers creams
- Nutritional supplements and hydration
- Minimize skin exposure to fecal, urinary, or any drainage.
Quiz Summary
0 of 5 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 5 Questions answered correctly
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- Current
- Review / Skip
- Answered
- Correct
- Incorrect
-
Question 1 of 5
1. Question
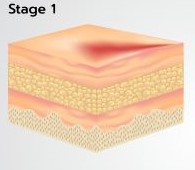
The new graduate nurse is caring for a client with a pressure ulcer like the one above. Which of the following statements by the new graduate nurses demonstrates that the nurse understands the proper nursing care for this pressure ulcer?
CorrectIncorrect -
Question 2 of 5
2. Question
Studies show that massaging the skin around this pressure ulcer promotes perfusion and healing.
CorrectIncorrect -
Question 3 of 5
3. Question
A stage 2 pressure sores needs to be left open to promote healing.
CorrectIncorrect -
Question 4 of 5
4. Question
Which of the following help promote tissue healing in pressure ulcers? Select all that apply
CorrectIncorrect -
Question 5 of 5
5. Question
Match the description with the stage of the ulcer.
Sort elements
- Full-thickness tissue loss. Subcutaneous fat may be visible
- Nonblanchable redness. Dermis Intact.
- Loss of dermis.
- Exposed bone, tendon or muscle
- Presence of eschar
-
Stage 3
-
Stage 1
-
Stage 2
-
Stage 4
-
Unstageable
CorrectIncorrect
