Diabetes
/*! elementor – v3.12.1 – 02-04-2023 */
.elementor-heading-title{padding:0;margin:0;line-height:1}.elementor-widget-heading .elementor-heading-title[class*=elementor-size-]>a{color:inherit;font-size:inherit;line-height:inherit}.elementor-widget-heading .elementor-heading-title.elementor-size-small{font-size:15px}.elementor-widget-heading .elementor-heading-title.elementor-size-medium{font-size:19px}.elementor-widget-heading .elementor-heading-title.elementor-size-large{font-size:29px}.elementor-widget-heading .elementor-heading-title.elementor-size-xl{font-size:39px}.elementor-widget-heading .elementor-heading-title.elementor-size-xxl{font-size:59px}
Diabetes Mellitus Type 1
/*! elementor – v3.12.1 – 02-04-2023 */
.elementor-accordion{text-align:left}.elementor-accordion .elementor-accordion-item{border:1px solid #d5d8dc}.elementor-accordion .elementor-accordion-item+.elementor-accordion-item{border-top:none}.elementor-accordion .elementor-tab-title{margin:0;padding:15px 20px;font-weight:700;line-height:1;cursor:pointer;outline:none}.elementor-accordion .elementor-tab-title .elementor-accordion-icon{display:inline-block;width:1.5em}.elementor-accordion .elementor-tab-title .elementor-accordion-icon svg{width:1em;height:1em}.elementor-accordion .elementor-tab-title .elementor-accordion-icon.elementor-accordion-icon-right{float:right;text-align:right}.elementor-accordion .elementor-tab-title .elementor-accordion-icon.elementor-accordion-icon-left{float:left;text-align:left}.elementor-accordion .elementor-tab-title .elementor-accordion-icon .elementor-accordion-icon-closed{display:block}.elementor-accordion .elementor-tab-title .elementor-accordion-icon .elementor-accordion-icon-opened,.elementor-accordion .elementor-tab-title.elementor-active .elementor-accordion-icon-closed{display:none}.elementor-accordion .elementor-tab-title.elementor-active .elementor-accordion-icon-opened{display:block}.elementor-accordion .elementor-tab-content{display:none;padding:15px 20px;border-top:1px solid #d5d8dc}@media (max-width:767px){.elementor-accordion .elementor-tab-title{padding:12px 15px}.elementor-accordion .elementor-tab-title .elementor-accordion-icon{width:1.2em}.elementor-accordion .elementor-tab-content{padding:7px 15px}}.e-con-inner>.elementor-widget-accordion,.e-con>.elementor-widget-accordion{width:var(–container-widget-width);–flex-grow:var(–container-widget-flex-grow)}
Cause
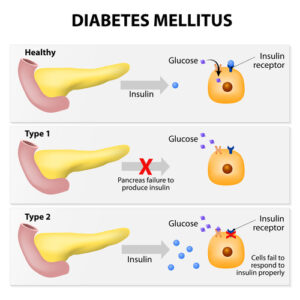 Beta cells of the pancreas DO NOT make insulin.
Beta cells of the pancreas DO NOT make insulin.- Autoimmune.
- Genetic.
- Diagnosed in childhood.
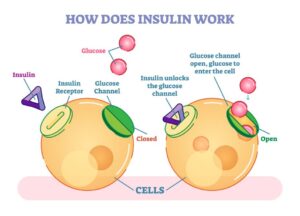
- No insulin to bring glucose into cells.
- Cells use alternative energy: fat and protein ⇒forming ketones and acidosis.
- Abrupt onset
Abrupt onset of symptoms in younger patients

- The P’s: Polydipsia, Polyphagia, Polyuria
- Also weight loss, fatigue, blurry vision and delayed wound healing.
 Insulin and only insulin
Insulin and only insulin- Oral medications will not work. Only life-long insulin
- Remember that pancreas does not produce insulin.
Diabetes Mellitus Type 2
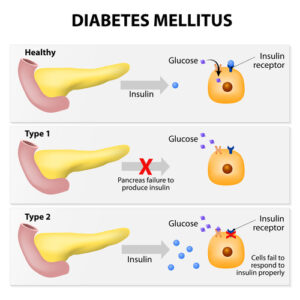 Pancreas produces some insulin, but insulin receptors DO NOT WORK properly.
Pancreas produces some insulin, but insulin receptors DO NOT WORK properly.- Insulin resistance.
- Diagnosed in adulthood
- Usually due to poor lifestyle (poor diet, no exercise, and obesity), smoking, family history, and sedentary lifestyle.
- Gradual onset in adulthood
- Sometimes asymptomatic or same symptoms as Type 1. Most dangerous since patient may not know and not get treatment for years.

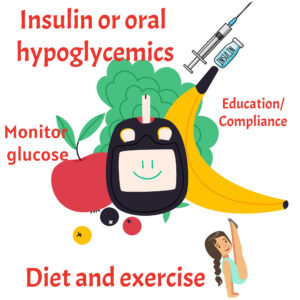
- Diet and exercise
- Oral hypoglycemic drugs such as glipizide and metformin
- Insulin if unable to control blood sugar with oral hypoglycemics
Diagnosing Diabetes
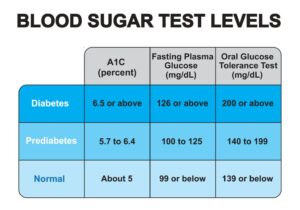 Random Blood Sugar > 200 mg/dl. I know table below does not show random blod sugar. But this is a great table to memorize.
Random Blood Sugar > 200 mg/dl. I know table below does not show random blod sugar. But this is a great table to memorize.
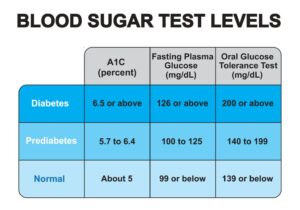 126 mg/dl after fasting for 8 hours
126 mg/dl after fasting for 8 hours
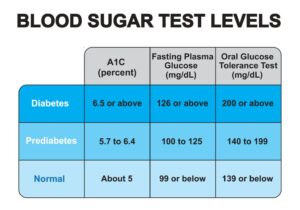 Blood sugar > 200mg/dl after ingesting 75 grams of glucose in water. Patient must be NPO. Glucose is taken before ingesting glucose and 2-3 times every 60 minutes.
Blood sugar > 200mg/dl after ingesting 75 grams of glucose in water. Patient must be NPO. Glucose is taken before ingesting glucose and 2-3 times every 60 minutes.
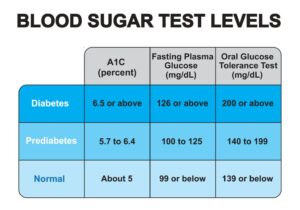 The A1C test measures what percentage of hemoglobin proteins in your blood are coated with sugar (glycated). Measures how well-controlled blood glucose levels have been over the past 2-3 MONTHS.
The A1C test measures what percentage of hemoglobin proteins in your blood are coated with sugar (glycated). Measures how well-controlled blood glucose levels have been over the past 2-3 MONTHS.
Insulin Complications
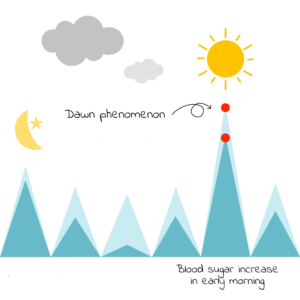
- Reduced sensitivity to insulin or surge of growth hormone at night that causes hyperglycemia before breakfast (5am to 8 am)
- Treatment: Increase bedtime dose of insulin. Dawn Phenomenon = Down insulin. DD

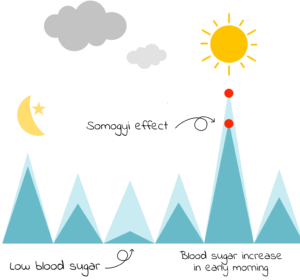
- Normal blood sugar at bedtime, but hypoglycemia occurs at about 03 am causing glucagon to be released and hyperglycemia occurs at 07 am.
- Treatment: Decrease bedtime insulin or increase bedtime snack
- Somogyi = 03 am hypoglycemia, need less insulin or more snack
- How to remember Somogyi=Somogyi So much insulin that we need to decrease.
Diabetes Complications
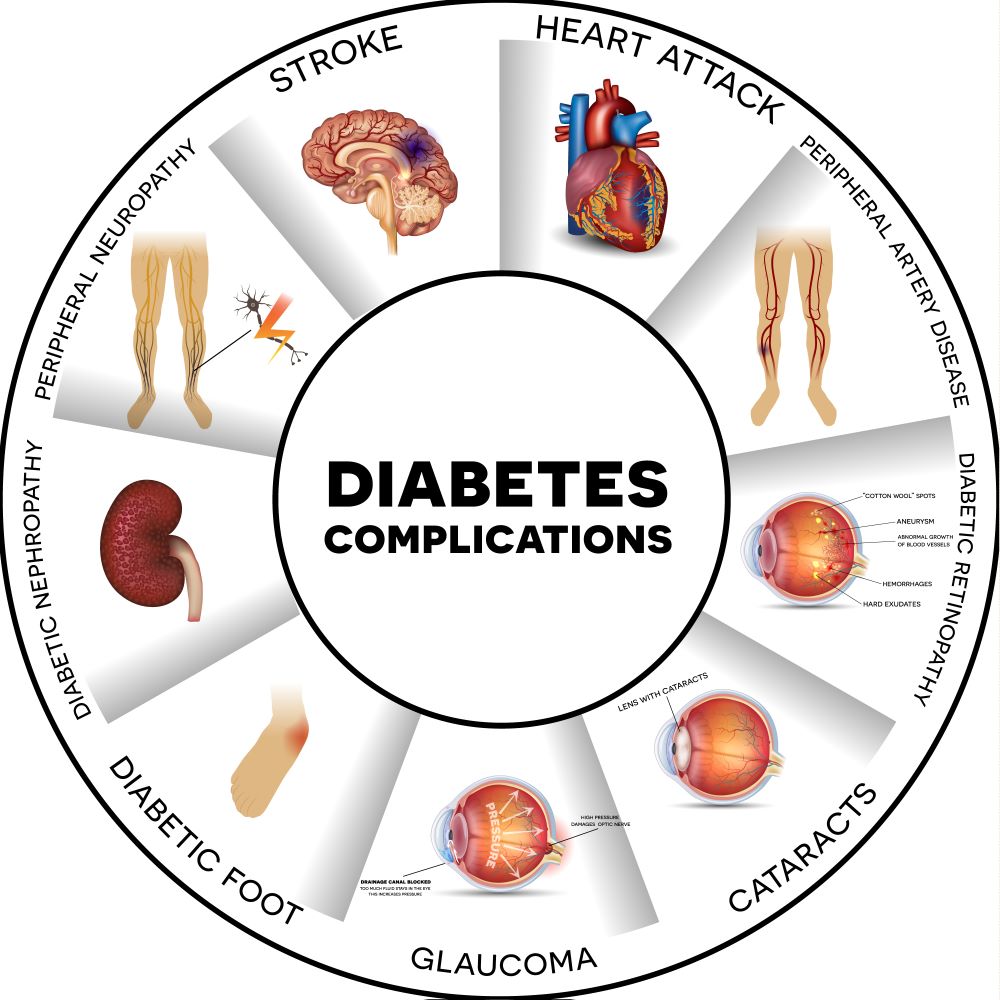
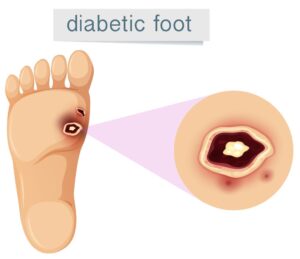 Pay special attention to feet. With peripheral neuropathy, patients may have a wound and not even feel it until it begins to turn into gangrene.
Pay special attention to feet. With peripheral neuropathy, patients may have a wound and not even feel it until it begins to turn into gangrene.
Surgical wounds may take longer to heal. Keep blood sugar under control. Even type 2 diabetics may need insulin when hospitalized.
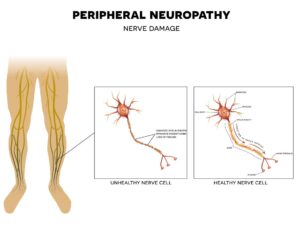 Hyperglycemia damages nerves
Hyperglycemia damages nerves
This causes numbness, tingling, and even loss of sensation.
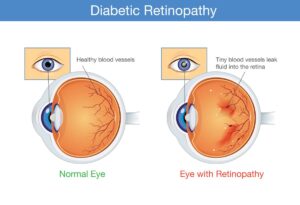 Hyperglycemia damages vessels of retina. Clients may also have glaucoma and cataracts.
Hyperglycemia damages vessels of retina. Clients may also have glaucoma and cataracts.
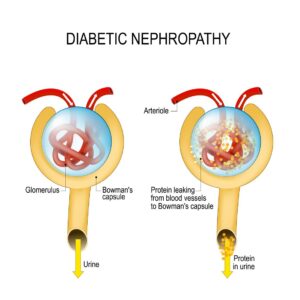 Hyperglycemia damages glomeruli
Hyperglycemia damages glomeruli
Diabetes is the second most common cause of end-stage renal disease. #1 = hypertension. Most clients with renal failure have both.
 Blockage of the blood vessels supplying the heart.
Blockage of the blood vessels supplying the heart.
 Cerebral Vascular Accident = Stroke
Cerebral Vascular Accident = Stroke
Foot Care
/*! elementor – v3.12.1 – 02-04-2023 */
.elementor-widget-image{text-align:center}.elementor-widget-image a{display:inline-block}.elementor-widget-image a img[src$=”.svg”]{width:48px}.elementor-widget-image img{vertical-align:middle;display:inline-block} 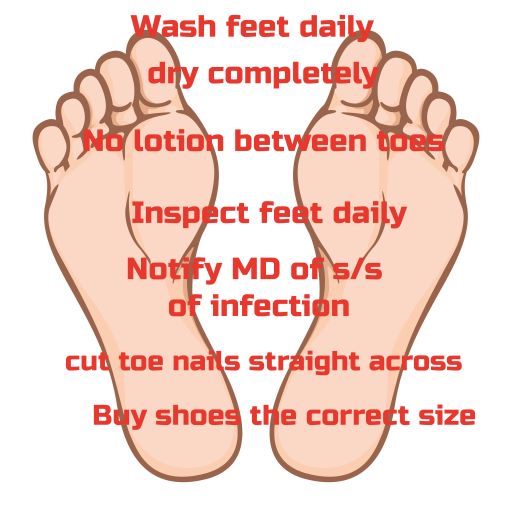
Inspect feet daily
- Use mirror if necessary
- check for cuts, blisters, or sores.
- Avoid Soaks
- Use warm water and mild soap
- Gently pat feet completely dry
BUT DO NOT APPLY BETWEEN TOES
Decreases circulation
- Never buy bigger shoes
- Buy shoes in the afternoon when feet are larger
- Have each foot measured every time you buy new shoes
- Buy leather shoes, not vinyl
Cut straight across
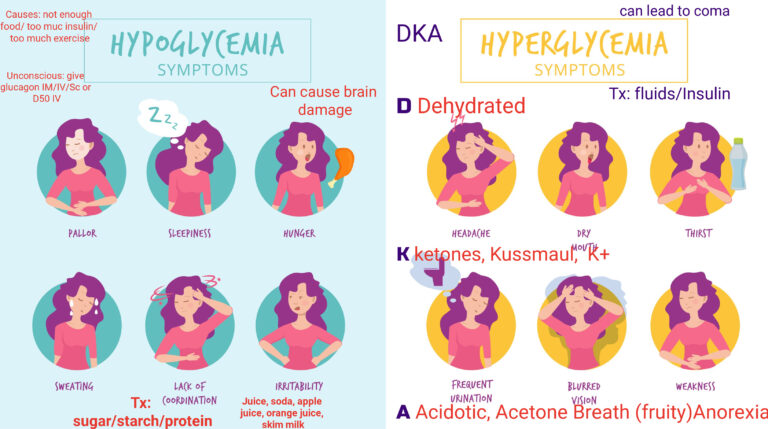
DKA vs HHNS
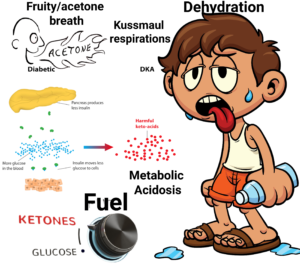
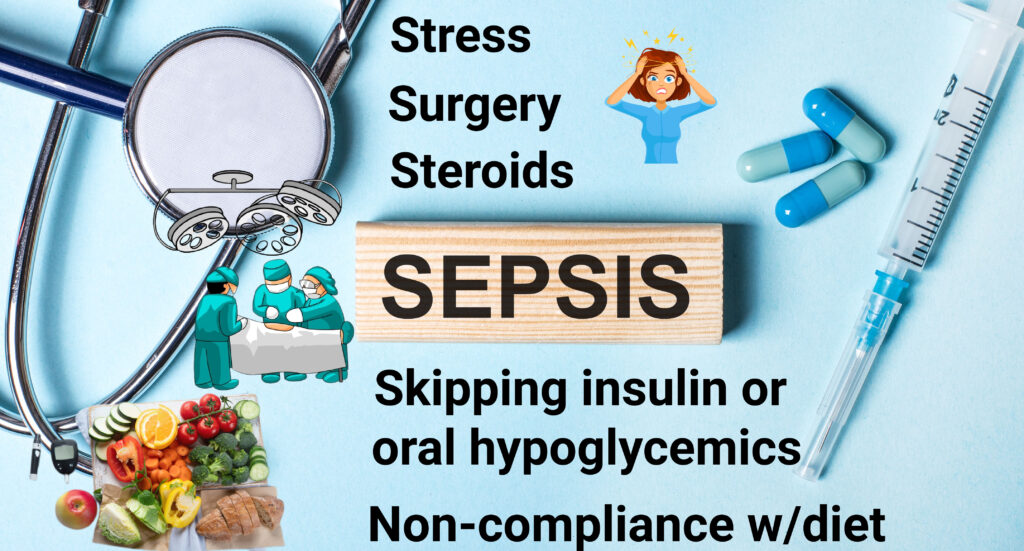
How Diabetic Ketoacidosis Develops
Low insulin prevents glucose from entering cells. Serum glucose becomes very high. The body starts to metabolize protein and fat into energy, which leads into ketones and acidosis
- Elevated glucose levels
- Dehydration
- Acidosis/Ketosis
- Kussmaul respirations: fast breathing to blow off acid. Lungs are trying to compensate for the metabolic acidosis
- Acetone/fruity breath
- Regular Insulin drip
- Hydration
- Correct electrolyte imbalances and acidosis
- Insulin drives K+ into the cell, so watch for hypokalemia
- Regular insulin is the ONLY insulin given IV
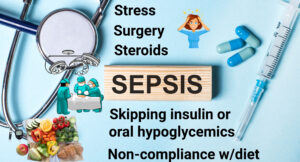
No acidosis and no ketones, but very high blood sugar
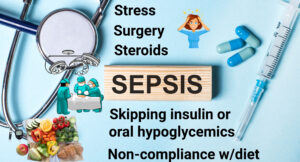
- Dehydration
- Infection
- Stress
- Decreased kidney function
- Dehydration
- Neuro changes (decreased LOC)
- No metabolic acidosis, no Kussmaul respirations
- Blood sugars can be very high (600+)
- Rehydration
- Correct electrolytes
- IV insulin with potassium replacement
Hyperglycemia vs. Hypoglycemia
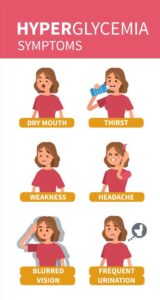
- All of the above plus. Ok, some repeat, but I want you to know them.
- Nausea/Vomiting
- Blurred vision/diplopia
- The 3 P’s. You better know them by now!
- Numbness
- Sugar in the urine (glycosuria)
The S’s again
 Diaphoresis (sweaty)
Diaphoresis (sweaty)- Palpitations
- Headache
- Irritability and Shakiness
- Fatigue
- Weakness
- Confusion
- Can lead to a coma and seizures without treatment
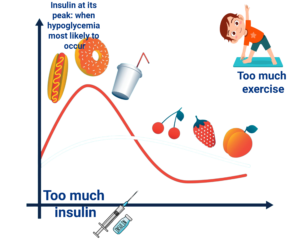
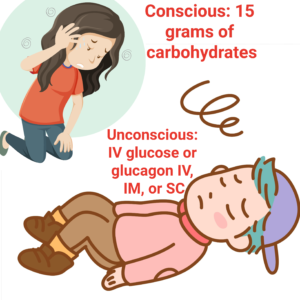 Dextrose 50% IV or Glucagon if unconscious.
Dextrose 50% IV or Glucagon if unconscious.
The different types of insulin
| Insulin | Onset | Peak | Duration | Some facts | When do you eat |
|---|---|---|---|---|---|
| Rapid-Acting (Aspart, Lispro, glulisine) Lispro = Humalog Glulisine = Apidra Aspart = Novolog | 15 minutes` | 30-90 minutes | 3-5 hours | At the same time of injection | |
| Short-Acting (Regular) | 30-60 minutes | 2-4 hours | 5-8 hours | Only insulin given IV | Within 30-60 minutes |
| Intermediate-Acting (NPH). Also called Isophane Insulin | 60-120 minutes | 4-12 hours | 14 hours | Can be mixed with Humalog, Novolog, and Regular. It is cloudy. Draw clear before cloudy; that is, Regular/Humalog/Novolog before NPH. Think RN (Regular before NPH). Given 2x/day | |
| Long-Acting (Detrimir, Lantus, and glargine) | 60-120 minutes | No Peak (Big question on NCLEX) | 24 hours | NEVER MIX |